Beyond the Average: Navigating Individual Variation in Drug Response for Precision Therapeutics
This article addresses the critical challenge of translating population-level data into effective treatments for individual patients in drug development.
Beyond the Average: Navigating Individual Variation in Drug Response for Precision Therapeutics
Abstract
This article addresses the critical challenge of translating population-level data into effective treatments for individual patients in drug development. It explores the foundational concepts of population means and individual variation, highlighting the limitations of a one-size-fits-all approach, as evidenced by the fact that over 99% of patients carry actionable pharmacogenomic variants. The content delves into advanced methodological frameworks like Population PK/PD and mixed-effects models designed to quantify and account for this variability. It further provides strategies for troubleshooting common issues in variability analysis and evaluates validation frameworks such as Individual and Population Bioequivalence. Aimed at researchers and drug development professionals, this article synthesizes insights from clinical pharmacology, statistics, and systems biology to chart a path toward more personalized and effective medical treatments.
The Myth of the Average Patient: Understanding Sources of Individual Variability
Defining Population Mean vs. Individual Variation in a Clinical Context
In clinical research and drug development, a fundamental tension exists between the population mean—the average treatment effect observed across a study cohort—and individual variation—the differences in how specific patients or subgroups respond to an intervention [1]. This distinction is not merely statistical but has profound implications for patient care, drug development, and healthcare policy. The population mean provides the foundational evidence for evidence-based medicine, yet clinicians treat individuals whose characteristics, risks, and treatment responses may differ significantly from the population average [2] [1]. Understanding this dichotomy is essential for interpreting clinical trial results, optimizing therapeutic interventions, and making informed decisions that balance collective evidence with individualized care.
Conceptual Framework: Populations and Individuals
Understanding the Population Mean
In clinical research, the term "population" is a theoretical concept encompassing all individuals sharing a particular set of characteristics or all potential outcomes of a specific treatment [2] [3]. The population mean (often denoted as μ) represents the average value of a measured outcome (e.g., reduction in blood pressure, survival rate) across this entire theoretical group. Crucially, this parametric mean is almost never known in practice because researchers cannot measure every member of the population [3]. Instead, they estimate it using the sample mean (x̄) calculated from a subset of studied patients.
The precision of this estimation depends heavily on sample size and variability. As sample size increases, sample means tend to cluster more closely around the true population mean due to the cancellation of random sampling errors [3]. This statistical phenomenon is quantified by the standard error of the mean (S.E.), which decreases as sample size increases and is estimated using the formula S.E. = s/√n, where s is the sample standard deviation and n is the sample size [3].
The Reality of Individual Variation
In contrast to population averages, individual variation reflects the diversity of treatment responses among patients due to differences in genetics, comorbidities, concomitant medications, lifestyle factors, and disease heterogeneity [1]. This variation presents a critical challenge for clinical decision-making, as the "average" treatment effect reported in trials may not accurately predict outcomes for individual patients.
The problem is exemplified by the re-analysis of the GUSTO trial, which compared thrombolytic drugs for heart attack patients [1]. While the overall population results showed t-PA was superior to streptokinase, this benefit was primarily driven by a high-risk subgroup. Lower-risk patients received minimal benefit from the more potent and risky drug, yet the population-level results led to widespread adoption of t-PA for all eligible patients [1]. This demonstrates how population means can obscure clinically important variation in treatment effects across patient subgroups.
Table 1: Key Terminology in Population vs. Individual Analysis
| Term | Definition | Clinical Interpretation |
|---|---|---|
| Population Mean | Average treatment effect across a theoretical population | Provides overall evidence for treatment efficacy; foundation for evidence-based medicine |
| Sample Mean | Average treatment effect observed in the studied patient sample | Estimate of population mean; precision depends on sample size and variability |
| Individual Variation | Differences in treatment response among individual patients | Explains why some patients benefit more than others from the same treatment |
| Standard Deviation | Measure of variability in individual patient outcomes | Quantifies the spread of individual responses around the mean |
| Standard Error | Measure of precision in estimating the population mean | Indicates how close the sample mean is likely to be to the true population mean |
Quantitative Comparisons: Effect Measures and Their Interpretation
Comparing Population Effect Measures
Clinical research employs various statistical measures to quantify treatment effects, each with distinct advantages and limitations for interpreting population-level versus individual-level implications [4]. Understanding these measures is essential for appropriate interpretation of clinical evidence.
Ratio measures, including risk ratios (RR), odds ratios (OR), and hazard ratios (HR), express the relative likelihood of an outcome occurring in the treated group compared to the control group [4]. These measures are useful for understanding the proportional benefit of a treatment but can be misleading because they communicate only relative differences rather than absolute differences. For example, an OR of 0.52 denotes a reduction of almost half in the risk of weaning in a breastfeeding intervention trial, but without knowing the baseline risk, the clinical importance is difficult to assess [4].
Absolute measures, particularly risk difference (RD), quantify the actual difference in risk between treated and untreated groups [4]. These measures are mathematically more intuitive and easier to interpret clinically. For instance, a study found that offering infants a pacifier once lactation was well established did not reduce exclusive breastfeeding at 3 months in a clinically meaningful way (RD = 0.004), meaning the percentage of exclusively breastfeeding babies at 3 months differed by only 0.4% [4].
Table 2: Comparison of Effect Measures in Clinical Research
| Effect Measure | Calculation | Interpretation | Example | Advantages | Limitations |
|---|---|---|---|---|---|
| Risk Ratio (RR) | Risk in exposed / Risk in unexposed | Relative difference in risk | RR=1.3: 30% increased risk in exposed | Easy to understand; commonly used | Does not reflect baseline risk; can exaggerate importance of small effects |
| Odds Ratio (OR) | Odds in exposed / Odds in unexposed | Relative difference in odds | OR=0.52: 48% reduction in odds | Useful for case-control studies; mathematically convenient | Often misinterpreted as risk ratio; less intuitive |
| Hazard Ratio (HR) | Hazard in exposed / Hazard in unexposed | Relative difference in hazard rates over time | HR=1.62: 62% increased hazard | Accounts for time-to-event data; uses censored observations | Requires proportional hazards assumption; complex calculation |
| Risk Difference (RD) | Risk in exposed - Risk in unexposed | Absolute difference in risk | RD=0.004: 0.4% absolute difference | Clinically intuitive; reflects actual risk change | Does not convey relative importance; depends on baseline risk |
Statistical Significance Versus Clinical Significance
A crucial distinction in interpreting clinical research is between statistical significance and clinical significance [4] [5] [6]. Statistical significance, conventionally defined by a p-value < 0.05, indicates that an observed effect is unlikely to be due to chance alone [4] [5]. However, statistical significance does not necessarily indicate that the effect is large enough to be clinically important.
Clinical significance denotes a difference in outcomes deemed important enough to create a lasting impact on patients, clinicians, or policy-makers [5]. The concept of minimal clinically important difference (MCID) represents "the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient's management" [5].
Alarmingly, contemporary research shows that most comparative effectiveness studies do not specify what they consider a clinically significant difference. A review of 307 studies found that only 8.5% defined clinical significance in their methods, yet 2.3% recommended changes in clinical decision-making, with 71.4% of these doing so without having defined clinical significance [5]. This demonstrates concerning over-reliance on statistical significance alone for clinical recommendations.
Experimental Approaches and Methodologies
Population Pharmacokinetic/Pharmacodynamic Modeling
Population pharmacokinetic/pharmacodynamic (PK/PD) modeling represents a sophisticated approach to understanding both population trends and individual variations in drug response [7]. This methodology uses non-linear mixed-effects modeling to characterize drug behavior while accounting for inter-individual variability.
In a study of the novel sedative HR7056, researchers developed a three-compartment model to describe its pharmacokinetics in Chinese healthy subjects [7]. The model included population mean parameters for clearance (1.49 L·min⁻¹), central volume (2.1 L), and inter-compartmental clearances (0.96 and 0.27 L·min⁻¹), while also quantifying inter-individual variability [7]. The pharmacodynamic component used a "link" model to relate plasma concentrations to effect-site concentrations and a sigmoid inhibitory effect model to describe the relationship between HR7056 concentration and its sedative effects measured by Bispectral Index (BIS) and Modified Observer's Assessment of Alertness/Sedation (MOAA/S) scores [7].
The structural model for the relationship between effect-site concentration (Ce) and drug effect (E) was described using the equation: E = E₀ - (Iₘₐₓ × Ceᵞ)/(IC₅₀ᵞ + Ceᵞ) where E₀ is the baseline effect, Iₘₐₓ is the maximum possible reduction in effect, IC₅₀ is the concentration producing 50% of maximum effect, and γ is the Hill coefficient describing curve steepness [7].
Subgroup and Risk-Based Analysis
An alternative approach to address individual variation involves conducting subgroup analyses based on patient risk profiles [1]. This method involves developing mathematical models to predict individual patient outcomes based on their characteristics, then analyzing treatment effects across different risk strata.
In the GUSTO trial re-analysis, researchers used a risk model to divide patients into quartiles based on their baseline mortality risk [1]. They discovered that the highest-risk quartile accounted for most of the mortality benefit that gave t-PA its advantage over streptokinase [1]. Similarly, in the ATLANTIS B trial of t-PA for stroke, risk stratification revealed that patients at lowest risk of thrombolytic-related hemorrhage actually benefited from t-PA treatment, even though the overall trial results showed no net benefit [1].
These approaches demonstrate how analyzing trial results through the lens of individual variation can reveal treatment effects masked by population-level analyses and provide clinicians with better tools for individualizing treatment decisions.
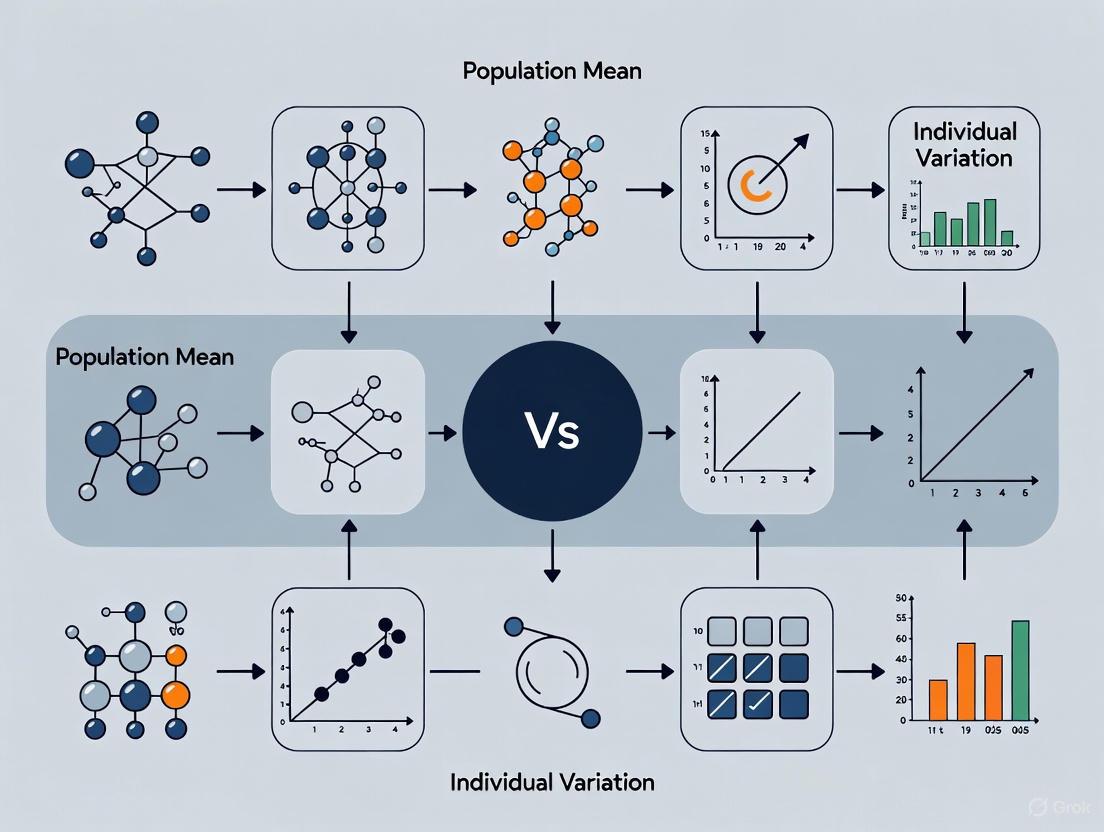
Visualizing the Relationship
The following diagram illustrates the conceptual relationship between population means and individual variation in clinical research, and how this relationship informs clinical decision-making:
Relationship Between Population and Individual Perspectives
Table 3: Research Reagent Solutions for Population and Individual Analysis
| Tool/Technique | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| Non-linear Mixed Effects Modeling | Estimate population parameters while quantifying inter-individual variability | Population PK/PD analysis | Requires specialized software (NONMEM, Phoenix NLME); complex implementation but powerful for sparse data |
| Risk Stratification Models | Identify patient subgroups with different treatment responses | Post-hoc analysis of clinical trials | Enhances clinical applicability but requires validation; risk of overfitting |
| Confidence Intervals | Quantify precision of effect estimates | Reporting of all clinical studies | Preferred over p-values alone; provide range of plausible values for true effect [4] |
| Minimal Clinically Important Difference | Define threshold for clinically meaningful effects | Study design and interpretation | Should be specified a priori; can use validated standards or clinical judgment [5] |
| Standard Error Calculation | Estimate precision of sample mean | Sample size planning and interpretation | S.E. = s/√n; decreases with larger sample sizes [3] |
The tension between population means and individual variation represents a fundamental challenge in clinical research and practice. Population means provide essential evidence for treatment efficacy and form the foundation of evidence-based medicine, but they inevitably obscure important differences in how individual patients respond to interventions. The contemporary over-reliance on statistical significance, without adequate consideration of clinical significance or individual variation, risks leading to suboptimal treatment decisions that may harm some patients while helping others.
Moving forward, clinical research should embrace methodologies that explicitly address both population-level effects and individual variation, including population PK/PD modeling, risk-based subgroup analysis, and consistent application of clinically meaningful difference thresholds. By better integrating these approaches, researchers and clinicians can develop more nuanced therapeutic strategies that respect both collective evidence and individual patient differences, ultimately advancing toward truly personalized medicine.
In the pursuit of personalized medicine, a fundamental statistical challenge lies in distinguishing true individual response to treatment from the background variability inherent in all biological systems. The common belief that there is a strong personal element in response to treatment is not always based on sound statistical evidence [8]. Research into personalized medicine relies on the assumption that substantial patient-by-treatment interaction exists, yet in almost all cases, the actual evidence for this is limited [9]. This guide compares how different experimental designs and statistical approaches succeed or fail at isolating three critical variance components: between-patient, within-patient, and patient-by-treatment interaction. Understanding these components is essential for drug development professionals aiming to determine whether treatments should be targeted to specific patient subgroups or applied more broadly.
Defining the Key Variance Components
In clinical trials, the observed variation in outcomes arises from multiple distinct sources. Statisticians formally account for these sources of variability to draw accurate conclusions about treatment effects [10]. The table below defines the four fundamental components of variance that must be understood and measured.
Table 1: Core Components of Variance in Clinical Trials
| Component of Variation | Statistical Definition | Clinical Interpretation |
|---|---|---|
| Between-Treatments (A) | Variation between treatments averaged over all patients [8] | The overall average effect of one treatment versus another |
| Between-Patient (B) | Variation between patients given the same treatments [8] | Differences in baseline severity, genetics, demographics, or comorbidities |
| Patient-by-Treatment Interaction (C) | Extent to which effects of treatments vary from patient to patient [8] | True individual response differences; the key to personalization |
| Within-Patient (D) | Variation from occasion to occasion when same patient is given same treatment [8] | Measurement error, temporal fluctuations, and environmental factors |
The relationship between these components can be visualized through the following conceptual framework:
Experimental Designs for Isolating Variance Components
Different clinical trial designs provide varying capabilities to isolate these variance components. The choice of design directly determines which components can be precisely estimated and which remain confounded.
Table 2: Identifiable Variance Components by Trial Design
| Trial Design | Description | Identifiable Components | Confounded "Error" Term |
|---|---|---|---|
| Parallel Group | Patients randomized to a single course of one treatment for the trial duration [8] | Between-Treatments (A) [8] | B + C + D [8] |
| Classical Cross-Over | Patients randomized to sequences of treatments, with each treatment studied in one period [8] | A, B [8] | C + D [8] |
| Repeated Period Cross-Over | Patients treated with each treatment in multiple periods with randomization [8] | A, B, C [8] | D [8] |
| N-of-1 Trials | Single patient undergoes multiple treatment periods with randomization in a replicated design [11] | Within-patient (D) for that individual | Minimal when properly replicated |
The workflow below illustrates how these designs progressively isolate variance components:
Case Study: Replicate Cross-Over Design
A compelling case study demonstrates how replicate cross-over designs can successfully isolate patient-by-treatment interaction [11]. In this methodology:
- Patient Recruitment: Participants undergo multiple treatment periods with randomized sequences
- Replication: Each treatment is administered multiple times to the same patient
- Measurement: Outcomes are measured consistently across all periods
- Statistical Analysis: Random-effects models partition variance into its components
This design represents a "lost opportunity" in drug development, as it enables formal investigation of where individual response to treatment may be important [11]. The essential materials required for implementing such designs include specialized statistical software capable of fitting mixed-effects models (such as R, SAS, or Python with appropriate libraries), validated outcome measurement instruments, randomization systems, and data collection protocols that minimize external variability.
Quantitative Methods for Assessing Heterogeneous Treatment Effects
Variance-Ratio Meta-Analysis
When cross-over designs are not feasible, the variance-ratio (VR) approach provides an alternative method for detecting heterogeneous treatment effects in parallel-group RCTs [12]. This method compares the variance of post-treatment scores between intervention and control groups.
Experimental Protocol for VR Analysis:
- Extract post-treatment standard deviations from both arms of RCTs
- Calculate variance ratio (VR): VR = σ²treatment / σ²control
- Combine VRs across studies using meta-analytic techniques
- Interpret results: VR > 1 suggests heterogeneous treatment effects
Application Example: In PTSD treatment research, VR meta-analysis revealed that psychological treatments showed greater outcome variance in treatment groups compared to control groups, suggesting possible treatment effect heterogeneity [12]. However, similar analyses for antipsychotics in schizophrenia and antidepressants in depression showed no evidence for heterogeneous treatment effects [12].
Marginal Structural Models for Drug Interactions
Advanced statistical methods like marginal structural models (MSMs) with inverse probability of treatment weighting (IPTW) can assess causal interactions between drugs using observational data [13].
Methodological Workflow:
- Data Collection: Gather electronic health records or claims data with quadruplets (D₁, D₂, X, Y) for drug exposures, covariates, and outcomes
- Variable Selection: Use elastic net or other methods to identify confounding variables
- Propensity Score Estimation: Model probability of treatment assignment given covariates
- Weighting: Apply inverse probability of treatment weights to create balanced pseudopopulations
- Model Fitting: Estimate causal parameters using weighted generalized linear models
Table 3: Comparison of Methods for Detecting Heterogeneous Treatment Effects
| Method | Study Design | Key Assumptions | Limitations |
|---|---|---|---|
| Repeated Cross-Over | Experimental | No carryover effects, stable patient condition over time [8] | Impractical for long-term outcomes, high cost and complexity |
| Variance-Ratio | Parallel-group RCTs | Equal baseline variances, normally distributed outcomes [14] | Cannot distinguish mediated effects from true interaction [14] |
| Marginal Structural Models | Observational | No unmeasured confounding, positivity, correct model specification [13] | Requires large sample sizes, sensitive to model misspecification |
Statistical Toolkit for Variance Component Analysis
The following tools and techniques form the essential "research reagent solutions" for investigating variance components in drug development:
Table 4: Essential Methodological Toolkit for Variance Component Analysis
| Tool Category | Specific Methods | Application Context |
|---|---|---|
| Experimental Designs | Repeated period cross-over, N-of-1 trials, Bayesian adaptive designs [8] [11] | Isolating patient-by-treatment interaction with maximal efficiency |
| Modeling Frameworks | Random-effects models, mixed models, marginal structural models, generalized estimating equations [8] [13] | Partitioning variance components while accounting for correlation structure |
| Causal Inference Methods | Inverse probability weighting, propensity score stratification, targeted maximum likelihood estimation [13] | Estimating treatment effect heterogeneity from observational data |
| Meta-Analytic Approaches | Variance-ratio meta-analysis, random-effects meta-regression [12] | Synthesizing evidence of heterogeneous treatment effects across studies |
Understanding these key statistical components has profound implications for pharmaceutical research and development. Between-patient variance highlights the importance of patient recruitment strategies and baseline assessments. Within-patient variance sets the lower bound for detecting meaningful treatment effects. Most critically, patient-by-treatment interaction represents the theoretical upper limit for personalization—if this component is minimal, then personalized treatment approaches have little margin for improvement [12].
Each variance component informs different aspects of drug development: between-patient variance affects trial sizing and stratification strategies; within-patient variance determines measurement precision requirements; and patient-by-treatment interaction dictates whether targeted therapies or companion diagnostics are viable development pathways. By applying the appropriate experimental designs and statistical methods outlined in this guide, researchers can make evidence-based decisions about when and how to pursue personalized medicine approaches rather than relying on assumptions about variable treatment response [8] [9].
For decades, drug development and dosage optimization have predominantly followed a "one-size-fits-all" approach, based on average response in the general population. This paradigm, focused on the population mean, fails to account for profound individual variation in drug metabolism and efficacy, often resulting in treatment failure or adverse drug reactions (ADRs) for substantial patient subsets [15]. Pharmacogenomics (PGx) has emerged as a transformative discipline that bridges this gap by studying how genetic variations influence individual responses to medications [16].
Recent evidence reveals a striking consensus: over 97% of individuals carry clinically actionable pharmacogenomic variants that significantly impact their response to medications [15] [17]. This article provides a comprehensive comparison of the experimental evidence supporting this conclusion, detailing the methodologies, technologies, and findings that are reshaping drug development and clinical practice toward a more personalized approach.
Quantitative Evidence: The Prevalence of Actionable Pharmacogenomic Variants Across Populations
Global and Regional Prevalence Studies
Table 1: Prevalence of Actionable PGx Variants Across Population Studies
| Population Cohort | Sample Size | % Carrying ≥1 Actionable Variant | Number of Pharmacogenes Analyzed | Key Genes with High Impact | Citation |
|---|---|---|---|---|---|
| Swiss Hospital Biobank | 1,533 | 97.3% | 13 | CYP2C19, CYP2D6, SLCO1B1, VKORC1 | [15] |
| General Swiss Population | 4,791 | Comparable to hospital cohort | 13 | CYP2C9, CYP2C19, CYP2D6, TPMT | [15] |
| Global 1000 Genomes | 2,504 | 55.4% carrying LoF variants | 120 | CYP2D6, CYP2C19, CYP2C9 | [18] |
| European PREPARE Study | 6,944 | >90% | 12 | CYP2C19, CYP2D6, SLCO1B1 | [17] |
| Mayo Clinic Pilot | 1,013 | 99% | 5 | CYP2D6, CYP2C19, CYP2C9, VKORC1, SLCO1B1 | [17] |
The consistency of these findings across diverse populations and methodologies is remarkable. The Swiss biobank study concluded that "almost all participants carried at least one actionable pharmacogenetic allele," with 31% of patients actually prescribed at least one drug for which they carried a high-risk variant [15]. The PREPARE study, the largest prospective clinical trial to date, further demonstrated the clinical utility of this knowledge, reporting a 30% decrease in adverse drug reactions when pharmacogenomic information guided prescribing [17].
Population-Specific Variant Frequencies
Table 2: Differentiated Allele Frequencies Across Major Populations
| Pharmacogene | Variant/Diplotype | Functional Effect | European Frequency | East Asian Frequency | African Frequency | Clinical Impact |
|---|---|---|---|---|---|---|
| CYP2C19 | *2, *3 (Poor Metabolizer) | Reduced enzyme activity | 25-30% | 40-50% | 15-20% | Altered clopidogrel, antidepressant efficacy [16] |
| CYP2D6 | *4 (Poor Metabolizer) | Reduced enzyme activity | 15-20% | 1-2% | 2-5% | Codeine, tamoxifen response [17] |
| CYP2D6 | Gene duplication (Ultra-rapid) | Increased enzyme activity | 3-5% | 1-2% | 10-15% | Risk of toxicity from codeine [17] |
| DPYD | HapB3 (rs56038477) | Reduced enzyme activity | 1-2% | 0.5-1% | 3-5% | Fluoropyrimidine toxicity [15] |
| SLCO1B1 | *5 (rs4149056) | Reduced transporter function | 15-20% | 10-15% | 1-5% | Simvastatin-induced myopathy [19] |
Population-specific differences in variant frequencies underscore why population mean approaches to drug dosing fail for many individuals. As one analysis noted, "racial and ethnic groups exhibit pronounced differences in the frequencies of numerous pharmacogenomic variants, with direct implications for clinical practice" [20]. For example, the CYP2C19*17 allele associated with rapid metabolism occurs in approximately 20% of Europeans but is less common in other populations, significantly affecting dosing requirements for proton pump inhibitors and antidepressants [16].
Methodological Approaches: Experimental Protocols for PGx Variant Detection
Next-Generation Sequencing Workflows
Figure 1: Next-Generation Sequencing PGx Analysis Workflow. The process transforms raw DNA data into clinically actionable recommendations through standardized bioinformatics steps.
The foundation of modern pharmacogenomics relies on next-generation sequencing (NGS) technologies that comprehensively characterize variation across pharmacogenes. A typical targeted NGS workflow includes:
DNA Isolation and Quality Control: High-molecular-weight DNA extraction, with quality verification via spectrophotometry and fluorometry [21].
Library Preparation and Target Enrichment: Fragmentation and adapter ligation followed by either:
- Hybridization capture using biotinylated probes targeting specific pharmacogenes
- Amplicon-based approaches using targeted PCR primers
- Targeted Adaptive Sampling with nanopore sequencing for real-time enrichment [17]
High-Throughput Sequencing: Using platforms such as:
- Illumina platforms (short-read)
- Oxford Nanopore Technologies (long-read)
- PacBio SMRT sequencing (long-read) [17]
Bioinformatic Analysis:
- Alignment to reference genome (GRCh37/38)
- Variant calling and quality filtering
- Star allele definition using tools like Aldy, PyPGx, or StellarPGx
- Diplotype assignment and phenotype prediction [22]
A 2024 study demonstrated that targeted adaptive sampling long-read sequencing (TAS-LRS) achieved 25x on-target coverage while simultaneously providing 3x off-target coverage for genome-wide variants, enabling accurate, haplotype-resolved testing of 35 pharmacogenes [17].
Genotyping Arrays and Functional Validation
For clinical applications focusing on known variants, genotyping arrays provide a cost-effective alternative:
- DNA Amplification and Fragmentation
- Hybridization to Custom Arrays containing probes for known PGx variants
- Fluorescence Detection and Genotype Scoring
- Functional Validation of novel variants via:
- In vitro enzyme activity assays using expressed recombinant enzymes
- Cell-based models to assess drug metabolism and transport
- Clinical pharmacokinetic studies correlating genotypes with drug exposure [21]
As highlighted in recent research, "stringent computational assessment methods and functional validation using experimental assays" are crucial for establishing the clinical validity of novel pharmacogenomic variants [21].
The Evolving PGx Landscape: Star Alleles and Clinical Interpretation
Dynamic Nature of Pharmacogenomic Nomenclature
Figure 2: Pharmacogenomic Clinical Interpretation Pipeline. Genetic variants are translated into clinical recommendations through standardized nomenclature systems and clinical guidelines.
The star allele nomenclature system provides standardized characterization of pharmacogene variants, but this system is highly dynamic. Analysis of PharmVar database updates reveals substantial evolution:
- 471 core alleles added between versions 1.1.9 and 6.2
- 49 core alleles redefined or removed during this period
- Updates impact clinical interpretation - 19.4% of diplotypes in reference datasets require revision [22]
This dynamic landscape necessitates regular updates to clinical decision support systems and genotyping algorithms to maintain accuracy. As one study concluded, "outdated allele definitions can alter therapeutic recommendations, emphasizing the need for standardized approaches including mandatory PharmVar version disclosure" [22].
Clinical Guideline Development
Consortia including the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetics Working Group (DPWG) have developed guidelines for over 100 gene-drug pairs with levels of evidence ranging from A-D [16] [19]. As of 2024, CPIC has published guidelines for 132 drugs with pharmacogenomic associations [19].
Research Reagent Solutions for Pharmacogenomic Studies
Table 3: Essential Research Tools for PGx Investigation
| Reagent/Resource | Category | Specific Examples | Research Application |
|---|---|---|---|
| Reference Materials | DNA Standards | GeT-RM samples, Coriell Institute collections | Assay validation, inter-laboratory comparison |
| Genotyping Arrays | Targeted Genotyping | PharmacoScan, Drug Metabolism Array, Custom Panels | Cost-effective screening of known PGx variants |
| Sequencing Panels | Targeted NGS | Illumina TruSight, Thermo Fisher PharmacoScan | Comprehensive variant detection in ADME genes |
| Bioinformatics Tools | Star Allele Callers | Aldy, PyPGx, StellarPGx, Stargazer | Diplotype assignment from sequencing data |
| Functional Assay Kits | Enzyme Activity | P450-Glo, Transporter Activity Assays | Functional validation of novel variants |
| Database Resources | Curated Knowledge | PharmGKB, PharmVar, CPIC Guidelines | Clinical interpretation, allele definitions |
These research tools enable comprehensive pharmacogenomic investigation from initial discovery to clinical implementation. The GeT-RM (Genetic Testing Reference Materials) program provides particularly valuable reference materials with experimentally validated genotypes for method validation and quality control [22].
The evidence is unequivocal: over 97% of individuals carry clinically actionable pharmacogenomic variants that significantly impact drug response. This reality fundamentally challenges the traditional population mean approach to drug development and dosing. The convergence of decreasing sequencing costs, standardized clinical guidelines, and robust evidence of clinical utility positions pharmacogenomics to transform therapeutic individualization.
Future directions include:
- Integration of rare variants into clinical prediction models
- Development of multi-gene panels for pre-emptive testing
- Implementation in electronic health records with clinical decision support
- Global expansion of population-specific pharmacogenomic resources
As one study aptly concluded, "implementing a genetically informed approach to drug prescribing could have a positive impact on the quality of healthcare delivery" [15]. The stark reality that actionable pharmacogenomic variants exist in the vast majority of patients represents both a challenge to traditional paradigms and an unprecedented opportunity for personalized medicine.
In the development and clinical application of pharmaceuticals, a fundamental tension exists between population-based dosing recommendations and individual patient response. The non-stimulant medication atomoxetine, used for attention-deficit/hyperactivity disorder (ADHD), exemplifies this challenge through its extensive pharmacokinetic variability primarily governed by the highly polymorphic cytochrome P450 2D6 (CYP2D6) enzyme. Population-derived averages for atomoxetine metabolism provide useful starting points for dosing, but individual genetic makeup can dramatically alter drug exposure, efficacy, and safety profiles.
Understanding this variability is crucial for drug development professionals and clinical researchers seeking to optimize therapeutic outcomes. The case of atomoxetine demonstrates how pharmacogenetic insights can bridge the gap between population means and individual variation, potentially informing both clinical practice and drug development strategies for medications metabolized by polymorphic enzymes.
The CYP2D6 Enzyme and Genetic Basis of Variability
CYP2D6 Genetic Architecture
The CYP2D6 gene, located on chromosome 22q13.2, encodes one of the most important drug-metabolizing enzymes in the cytochrome P450 superfamily, responsible for metabolizing approximately 25% of all marketed drugs [23]. This gene exhibits remarkable polymorphism, with over 135 distinct star (*) alleles identified and cataloged by the Pharmacogene Variation (PharmVar) Consortium [24]. These alleles result from single nucleotide polymorphisms, insertions/deletions, and copy number variations, which collectively determine an individual's metabolic capacity for CYP2D6 substrates.
- Normal function alleles: *1, *2, *35 (Activity score = 1)
- Decreased function alleles: *9, *17, *29, *41 (Activity score = 0.5)
- Severely decreased function alleles: *10 (Activity score = 0.25)
- No function alleles: *3, *4, *5, *6, *40 (Activity score = 0)
- Increased function alleles: Gene duplications (e.g., *1x2, *2x2) (Activity score = 2 per copy)
Phenotype Classification System
The combination of CYP2D6 alleles (diplotype) determines metabolic phenotype through an activity score system recommended by the Clinical Pharmacogenetics Implementation Consortium (CPIC) [24]:
- Poor Metabolizers (PM): Activity score = 0 (No functional enzyme activity)
- Intermediate Metabolizers (IM): Activity score = 0.25-1.0 (Reduced enzyme activity)
- Normal Metabolizers (NM): Activity score = 1.25-2.25 (Standard enzyme activity)
- Ultrarapid Metabolizers (UM): Activity score > 2.25 (Enhanced enzyme activity)
Population Distribution of CYP2D6 Phenotypes
The frequency of CYP2D6 phenotypes exhibits substantial interethnic variation, with important implications for global drug development and dosing strategies [24]. Normal and intermediate metabolizers represent the most common phenotypes across populations, but poor and ultrarapid metabolizers constitute significant minorities at higher risk for adverse drug reactions or therapeutic failure.
Table 1: Global Distribution of CYP2D6 Phenotypes
| Population | Poor Metabolizers (%) | Intermediate Metabolizers (%) | Normal Metabolizers (%) | Ultrarapid Metabolizers (%) |
|---|---|---|---|---|
| European | 5-10% | 10-44% | 43-67% | 3-5% |
| Asian | ~1% | 39-46% | 48-52% | 0-1% |
| African | ~2% | 25-35% | 50-60% | 5-10% |
| Latino | 2-5% | 30-40% | 50-60% | 2-5% |
Atomoxetine Pharmacokinetics and CYP2D6-Mediated Metabolism
Metabolic Pathway of Atomoxetine
Atomoxetine undergoes extensive hepatic metabolism primarily via the CYP2D6 pathway, resulting in formation of its major metabolite, 4-hydroxyatomoxetine, which is subsequently glucuronidated [25]. In CYP2D6 normal metabolizers, atomoxetine has an absolute bioavailability of approximately 63% due to significant first-pass metabolism, compared to 94% in poor metabolizers who lack functional CYP2D6 enzyme activity [25]. This metabolic difference fundamentally underpins the substantial variability in drug exposure observed across different CYP2D6 phenotypes.
Magnitude of Exposure Variability
Research has consistently demonstrated that CYP2D6 polymorphism results in profound differences in atomoxetine pharmacokinetics. Studies report 8-10-fold higher systemic exposure (AUC) in CYP2D6 poor metabolizers compared to extensive metabolizers following identical dosing [25]. In clinical practice, this variability can extend up to 25-fold differences in plasma concentrations between individuals with different CYP2D6 phenotypes receiving the same weight-adjusted dose [26]. This exceptional range of exposure represents one of the most dramatic examples of pharmacogenetically-determined pharmacokinetics in clinical medicine.
Table 2: Atomoxetine Pharmacokinetic Parameters by CYP2D6 Phenotype
| Parameter | Poor Metabolizers | Normal Metabolizers | Ultrarapid Metabolizers |
|---|---|---|---|
| Bioavailability | 94% | 63% | Reduced |
| AUC | 8-10 fold higher | Reference | Reduced |
| Cmax | Higher | Reference | Lower |
| Tmax | 2.5 hours | 1.0 hour | Similar to NM |
| Half-life | 21.6 hours | 5.2 hours | Shorter |
| Clearance | Significantly reduced | Reference | Increased |
Experimental Evidence and Clinical Correlations
CYP2D6 Genotype and Dosing Response Relationships
A 2024 double-blind crossover study examining ADHD treatment response investigated relationships between CYP2D6 phenotype and atomoxetine efficacy over a 4-week period [27]. The results identified statistically significant trends in how CYP2D6 phenotype modified the time-response relationship for ADHD total symptoms (p = 0.058 for atomoxetine). Additionally, the dopamine transporter gene (SLC6A3/DAT1) 3' UTR VNTR genotype showed evidence of modifying dose-response relationships for atomoxetine (p = 0.029), suggesting potential pharmacodynamic influences beyond the pharmacokinetic effects of CYP2D6.
Therapeutic Drug Monitoring and Clinical Outcomes
A comprehensive 2024 retrospective study of 385 children with ADHD provided critical insights into the relationship between CYP2D6 genotype, plasma atomoxetine concentrations, and clinical outcomes [26]. The investigation revealed that CYP2D6 intermediate metabolizers exhibited 1.4-2.2-fold higher dose-corrected plasma atomoxetine concentrations compared to extensive metabolizers. Furthermore, intermediate metabolizers demonstrated a significantly higher response rate (93.55% vs. 85.71%, p = 0.0132) with higher peak plasma concentrations.
Receiver operating characteristic (ROC) analysis established that patients receiving once-daily morning dosing exhibited more effective response when plasma atomoxetine concentrations reached ≥268 ng/mL (AUC = 0.710, p < 0.001) [26]. The study also identified concentration thresholds for adverse effects, with intermediate metabolizers experiencing more central nervous system and gastrointestinal adverse reactions at plasma concentrations of 465 ng/mL and 509 ng/mL, respectively.
Comparative Efficacy Across Metabolizer States
Research has demonstrated that while CYP2D6 genotype significantly influences atomoxetine pharmacokinetics, most children with ADHD who are CYP2D6 normal metabolizers or have specific DAT1 genotypes (10/10 or 9/10 repeats) respond well to both atomoxetine and methylphenidate after appropriate dose titration [27]. However, the trajectory of response differs across metabolizer states, with poor and intermediate metabolizers achieving therapeutic concentrations more rapidly at lower doses, while ultrarapid metabolizers may require higher dosing or alternative dosing strategies to achieve efficacy.
Research Methodologies for Investigating CYP2D6-Atomoxetine Relationships
Population Pharmacokinetic Modeling Approaches
Population pharmacokinetics has emerged as a powerful methodology for quantifying and explaining variability in drug exposure [28] [29]. Unlike traditional pharmacokinetic studies that intensively sample small numbers of healthy volunteers, population approaches utilize sparse data collected from patients undergoing treatment, enabling identification of covariates that influence drug disposition.
The mixed-effects modeling approach fundamental to population pharmacokinetics incorporates:
- Fixed effects: Structural model parameters (e.g., clearance, volume of distribution) and demographic/clinical factors that significantly influence pharmacokinetics (e.g., weight, genotype)
- Random effects: Variance model parameters including intersubject variability and residual unexplained variability
This methodology allows researchers to pool data from multiple sources with varying dosing regimens and sampling times, making it particularly valuable for studying special populations where intensive sampling is impractical [29].
Genotype-Guided Clinical Trial Design
Contemporary investigations of CYP2D6-atomoxetine relationships typically incorporate prospective genotyping with stratified enrollment to ensure representation across metabolizer phenotypes [27] [26]. The essential protocol elements include:
- Genotyping Methodologies: Targeted amplification followed by sequencing, microarray analysis, or real-time PCR for key CYP2D6 variant alleles
- Phenotype Assignment: Translation of diplotype to activity score and phenotype category using standardized CPIC guidelines
- Pharmacokinetic Sampling: Strategic sampling at steady-state with precise documentation of dosing-to-sampling intervals
- Clinical Outcome Assessment: Standardized rating scales (e.g., ADHD-RS, IVA-CPT) administered at baseline and following treatment initiation
- Therapeutic Drug Monitoring: Correlation of plasma concentrations with both efficacy and adverse effect endpoints
Integrated Pharmacogenetic-Pharmacodynamic Modeling
Advanced research approaches now integrate CYP2D6 genotyping with therapeutic drug monitoring and clinical response assessment to develop comprehensive exposure-response models [26]. These models account for both the pharmacokinetic variability introduced by CYP2D6 polymorphism and potential pharmacodynamic modifiers such as the dopamine transporter (SLC6A3/DAT1) genotype, enabling more precise prediction of individual patient response to atomoxetine therapy.
Visualization of Atomoxetine Metabolism and Research Workflow
Atomoxetine Metabolic Pathway
Atomoxetine Metabolic Pathway: This diagram illustrates the primary metabolic pathway of atomoxetine, highlighting the crucial role of CYP2D6 in converting the parent drug to its hydroxylated metabolite prior to elimination.
Research Methodology Workflow
Pharmacogenomic Research Workflow: This flowchart outlines the comprehensive methodology for investigating CYP2D6-atomoxetine relationships, integrating genotyping, therapeutic drug monitoring, and clinical outcome assessment.
Table 3: Essential Research Materials for CYP2D6-Atomoxetine Investigations
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Genotyping Technologies | TaqMan allelic discrimination assays, PCR-RFLP, sequencing panels, microarrays | CYP2D6 allele definition and diplotype assignment |
| Analytical Instruments | LC-MS/MS systems, HPLC-UV | Quantification of plasma atomoxetine and metabolite concentrations |
| Clinical Assessment Tools | ADHD-RS, IVA-CPT, Conners' Rating Scales | Objective measurement of treatment efficacy and symptom improvement |
| Pharmacokinetic Software | NONMEM, Phoenix NLME, Monolix | Population PK modeling and covariate analysis |
| Reference Materials | PharmVar CYP2D6 allele definitions, CPIC guidelines | Standardized genotype to phenotype translation and dosing recommendations |
| Biobanking Resources | DNA extraction kits, blood collection tubes, temperature-controlled storage | Sample management for retrospective and prospective analyses |
Clinical Implementation and Dosing Recommendations
CPIC Guideline Recommendations
The Clinical Pharmacogenetics Implementation Consortium has established evidence-based guidelines for atomoxetine dosing based on CYP2D6 genotype [30] [31]. These recommendations represent the formal translation of pharmacogenetic research into clinical practice:
- Poor Metabolizers: Consider initiating with 50% of the standard dose and titrate to efficacy or maximum plasma concentrations of approximately 400 ng/mL
- Intermediate Metabolizers: Initiate with standard dosing but consider slower titration with therapeutic drug monitoring
- Normal Metabolizers: Standard dosing recommendations apply with routine monitoring
- Ultrarapid Metabolizers: May require higher doses (up to 1.8 mg/kg/day) to achieve therapeutic exposure
Therapeutic Drug Monitoring Targets
Based on recent evidence, the following plasma concentration thresholds have been proposed for optimizing atomoxetine therapy [26]:
- Efficacy Threshold: ≥268 ng/mL for patients receiving once-daily morning dosing
- CNS Adverse Effects: ≥465 ng/mL in intermediate metabolizers
- GI Adverse Effects: ≥509 ng/mL in intermediate metabolizers
These thresholds highlight the importance of considering both genotype and drug concentrations when individualizing atomoxetine therapy.
The case of CYP2D6 genotype and atomoxetine exposure provides a compelling illustration of the critical tension between population means and individual variation in drug development and clinical practice. While population averages provide essential starting points for dosing recommendations, the 25-fold variability in atomoxetine exposure mediated by CYP2D6 polymorphism necessitates a more personalized approach.
The integration of pharmacogenetic testing, therapeutic drug monitoring, and population pharmacokinetic modeling offers a powerful framework for optimizing atomoxetine therapy across diverse patient populations. This case study underscores the importance of incorporating pharmacogenetic principles throughout the drug development process, from early clinical trials through post-marketing surveillance, to ensure both efficacy and safety in the era of precision medicine.
For drug development professionals, the atomoxetine example demonstrates the value of prospective pharmacogenetic screening in clinical trials and the importance of considering genetic polymorphisms when establishing dosing recommendations for medications metabolized by polymorphic enzymes. As pharmacogenetics continues to evolve, this approach promises to enhance therapeutic outcomes across numerous drug classes and clinical indications.
A fundamental challenge in modern pharmacology lies in the critical difference between the population average and individual patient response. While drug development and regulatory decisions often focus on the doses that are, on average, safe and effective for a population, the reality is that "many individuals possess characteristics that make them unique" [32]. This inter-individual variability means that a fixed dose can result in a wide range of drug exposures and therapeutic outcomes across different patients. Non-genetic factors—including age, organ function, drug interactions, and lifestyle—constitute major sources of this variability, profoundly influencing drug disposition and effects. Understanding these contributors is essential for moving beyond the "average patient" model and toward more precise, individualized therapeutic strategies that account for the complete physiological context of each patient [32].
The Impact of Aging on Pharmacokinetics and Pharmacodynamics
Physiological Changes with Aging
Aging is a multifaceted physiological process characterized by the progressive decline in the function of various organ systems. It involves a "gradual loss of cellular function and the systemic deterioration of multiple tissues," which increases susceptibility to age-related diseases [33]. At the molecular level, aging is associated with several hallmarks, including genomic instability, telomere attrition, epigenetic alterations, and mitochondrial dysfunction, which collectively contribute to the overall functional decline [33] [34]. This decline manifests as a reduced homeostatic capacity, making it more challenging for older adults to maintain physiological balance under stress, including the stress imposed by medication regimens [35].
Pharmacokinetic (PK) Changes in the Elderly
Pharmacokinetics, which encompasses the processes of drug absorption, distribution, metabolism, and excretion (ADME), undergoes significant changes with advancing age. Table 1 summarizes the key age-related physiological changes and their impact on drug PK.
Table 1: Age-Related Physiological Changes and Their Pharmacokinetic Impact
| Pharmacokinetic Process | Key Physiological Changes with Aging | Impact on Drug Disposition | Clinical Implications |
|---|---|---|---|
| Absorption | Decreased gastric acidity; Delayed gastric emptying; Reduced splanchnic blood flow [35] | Minimal clinical change for most drugs; Potential alteration for drugs requiring acidic environment or active transport [35] | Generally, no dose adjustment solely for absorption changes. |
| Distribution | ↑ Body fat (20-40%); ↓ Lean body mass (10-15%); ↓ Total body water [35] | ↑ Volume of distribution for lipophilic drugs (e.g., diazepam); ↓ Volume of distribution for hydrophilic drugs (e.g., digoxin) [35] | Lipophilic drugs have prolonged half-lives; hydrophilic drugs achieve higher plasma concentrations. |
| Metabolism | Reduced hepatic mass and blood flow; Variable changes in cytochrome P450 activity [35] | ↓ Hepatic clearance for many drugs; Increased risk of drug accumulation [35] | Dose reductions often required for hepatically cleared medications. |
| Excretion | ↓ Renal mass and blood flow; ↓ Glomerular filtration rate (GFR) [35] | ↓ Renal clearance for drugs and active metabolites [35] | Crucial to estimate GFR and adjust doses of renally excreted drugs. |
Pharmacodynamic (PD) Changes in the Elderly
Pharmacodynamics, which describes the body's biological response to a drug, also alters with age. Older patients often exhibit increased sensitivity to various drug classes, even at comparable plasma concentrations [35]. For instance, they experience heightened effects from central nervous system (CNS)-active drugs like benzodiazepines, leading to more pronounced sedation and impaired performance [35]. This increased sensitivity may stem from factors such as "loss of neuronal substance, reduced synaptic activity, impaired brain glucose metabolism, and rapid drug penetration into the central nervous system" [35]. Conversely, older adults can also demonstrate decreased sensitivity to some drugs, such as a weakened cardiac response to β-agonists like dobutamine due to changes in β-adrenergic receptor sensitivity [35]. These PD changes, combined with PK alterations, significantly increase the vulnerability of older adults to adverse drug reactions (ADRs).
Drug-Drug and Drug-Lifestyle Interactions
Polypharmacy as a Prevalent Risk Factor
Polypharmacy, commonly defined as the concurrent use of five or more medications, is a global healthcare concern, especially among the elderly [36]. It poses significant challenges, leading to "medication non-adherence, increased risk of drug duplication, drug–drug interactions, and adverse drug reactions (ADRs)" [36]. ADRs are a leading cause of mortality in developed countries, and polypharmacy is a key contributor to this risk. A study analyzing 483 primarily elderly and polymedicated patients found that the most frequently prescribed drug classes included antihypertensives, platelet aggregation inhibitors, cholesterol-lowering drugs, and gastroprotective agents [36]. The complex medication regimens increase the probability of interactions, which can be pharmacokinetic (affecting drug levels) or pharmacodynamic (affecting drug actions).
The Role of Lifestyle Factors
Lifestyle factors, including diet, smoking, alcohol consumption, exercise, and sleep, are recognized modifiable contributors to biological aging and drug response variability [37]. These factors can directly and indirectly influence drug efficacy and safety. For example, dietary components can inhibit or induce drug-metabolizing enzymes, while smoking can induce CYP1A2 activity, increasing the clearance of certain drugs [36]. A large longitudinal cohort study in Southwest China demonstrated that healthy lifestyle changes, particularly improvements in diet and smoking cessation, were inversely associated with accelerated biological aging across multiple organ systems [37]. The study found that diet was the major contributor to slowing comprehensive biological aging (24%), while smoking cessation had the greatest impact on slowing metabolic aging (55%) [37]. This underscores the powerful role lifestyle plays in modulating an individual's physiological state and, consequently, their response to pharmacotherapy.
Methodologies for Studying Non-Genetic Variability
Population Pharmacokinetic (PopPK) Modeling
To quantify and account for variability in drug exposure, researchers employ population pharmacokinetic (PopPK) methods. Unlike traditional PK analyses that require dense sampling from each individual, PopPK uses sparse data collected from a population of patients to identify and quantify sources of variability [38]. The standard approach is Non-linear Mixed Effects Modeling (NONMEM), which involves:
- Developing a Structural Model: A model that best describes the absorption, distribution, and elimination of the drug, characterizing the population mean concentration-time curve [38].
- Identifying Covariates: Systematic exploration of patient factors (covariates) that explain variability in PK parameters. Covariates examined typically include age, body size, and measures of renal and hepatic function [38].
- Quantifying Random Variability: The model distinguishes between inter-individual variability (IIV), inter-occasion variability, and residual unexplained variability [38] [39].
This approach allows for the development of models that can predict drug exposure in individuals with specific demographic and physiological characteristics.
Advanced Preclinical Models
Incorporating patient diversity early in drug development is crucial for predicting clinical outcomes. Advanced preclinical models, such as 3D microtissues derived from a range of human donors, are being used to address this need [40]. Unlike traditional 2D cell cultures or animal models, these platforms can maintain key physiological features and be produced using cells from multiple individuals with unique genetic and metabolic profiles [40]. This capability enables drug developers to:
- Uncover inter-individual variability in drug response and toxicity.
- De-risk clinical trials by providing a clearer picture of how a drug might perform in diverse populations.
- Tailor therapies for personalized medicine by evaluating biomarkers and other factors relevant to patient stratification [40].
Bioequivalence and Interchangeability
When evaluating generic drugs or new formulations, bioequivalence studies are critical. The concept extends beyond simple average bioequivalence, which only compares average bioavailability [41]. To fully assess interchangeability, more robust methods are used:
- Population Bioequivalence: Assesses the total variability of the bioavailability measure in the population, ensuring that a prescriber can confidently choose either the test or reference product for a new patient [41].
- Individual Bioequivalence: Assesses within-subject variability for the test and reference products, ensuring that a patient can be safely switched from one product to another [41]. These statistical approaches ensure that not only the average exposure but also the variability in exposure is comparable between products, safeguarding therapeutic equivalence across a diverse patient population.
Experimental Data and Supporting Evidence
Quantitative Data on Drug Utilization and Interactions
Data from a study of 483 elderly, polymedicated patients provides concrete evidence of the complex medication landscape in this population. Table 2 lists the most frequently used drug classes and their prevalence, highlighting the high potential for drug-drug interactions [36].
Table 2: Most Frequently Used Drug Classes in an Elderly Polymedicated Cohort (n=483) [36]
| Drug/Treatment Class | Frequency of Use (%) | Male Frequency of Use (%) | Female Frequency of Use (%) |
|---|---|---|---|
| Antihypertensives | 72.26% | 78.60% | 67.16% |
| Platelet aggregation inhibitors/anticoagulants | 65.84% | 68.37% | 63.81% |
| Cholesterol-lowering drugs | 55.49% | 56.74% | 54.48% |
| Gastroprotective agents | 52.17% | 50.23% | 53.73% |
| Sleep disorder treatment | 34.78% | 24.19% | 43.28% |
| Diuretics | 32.92% | 32.56% | 33.21% |
| Analgesics | 32.30% | 22.33% | 40.30% |
| Anxiolytics | 30.85% | 20.47% | 39.18% |
The same study also analyzed drug-lifestyle interactions, finding that these primarily involved inhibitions but also included inductions of metabolic pathways, with significant differences observed when analyzed by gender [36].
Protocol for PopPK Analysis
A detailed protocol for conducting a PopPK analysis to estimate within-subject variability (WSV) using single-period clinical trial data is as follows [39]:
- Data Collection: Administer the drug of interest to a cohort of subjects (≥18 subjects recommended for reliable estimation) and collect plasma samples at scheduled time points.
- Bioanalytical Assay: Quantify drug concentrations in the plasma samples using a validated method (e.g., LC-MS/MS) to ensure data quality and minimize assay-related variability.
- Model Development: Using NONMEM software:
- Input the concentration-time data for all subjects.
- Develop a structural PK model (e.g., one- or two-compartment) to describe the drug's disposition.
- Estimate the fixed effects (typical PK parameters like clearance and volume of distribution) and random effects (IIV and residual variability).
- Model Validation: Evaluate the model's performance using diagnostic plots and statistical criteria. The estimated residual variability (RV) in a well-controlled study approximates the WSV.
- Data Application: The estimated WSV can then be used for more accurate sample size calculation in future clinical trials, ensuring they are neither underpowered nor ethically and economically inefficient due to excessive subject numbers [39].
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Research Tools for Studying Non-Genetic Variability
| Tool/Reagent | Function/Application |
|---|---|
| Population PK Software (e.g., NONMEM) | The industry standard for non-linear mixed-effects modeling, used to perform PopPK analyses and quantify IIV and RV from sparse clinical data [38] [39]. |
| 3D In Vitro Microtissue Platforms | Physiologically relevant models derived from primary human cells from multiple donors; used to assess inter-individual variability in drug response, metabolism, and toxicity during preclinical development [40]. |
| Validated Bioanalytical Assays (e.g., LC-MS/MS) | Essential for the accurate quantification of drug and metabolite concentrations in biological fluids (plasma, serum), providing the high-quality data required for PK and PopPK analyses [39]. |
| Clinical Data Management System | Secure software for managing and integrating complex clinical trial data, including demographic information, laboratory values, medication records, and PK sampling times. |
| Cocktail Probe Substrates | A set of specific drugs each metabolized by a distinct enzyme pathway; administered to subjects to simultaneously phenotype multiple drug-metabolizing enzyme activities in vivo. |
Integrated Pathways of Non-Genetic Variability
The following diagram synthesizes the interconnected pathways through which non-genetic factors contribute to variability in individual drug response, framing it within the conflict between population mean and individual patient needs.
Diagram: Pathways Linking Non-Genetic Factors to Variable Drug Response. The diagram illustrates how non-genetic factors create variability from the population mean, necessitating precision medicine approaches.
The journey from population-based dosing to truly individualized therapy requires a deep understanding of non-genetic sources of variability. Age-related physiological changes, declining organ function, complex drug interactions, and modifiable lifestyle factors collectively exert a powerful influence on drug pharmacokinetics and pharmacodynamics, often overshadowing the "average" profile derived from clinical trials. Tackling this complexity demands robust methodological tools—such as population PK modeling, advanced in vitro systems, and comprehensive bioequivalence assessments—that can quantify and integrate these factors. By systematically accounting for the contributors outlined in this guide, researchers and drug developers can better navigate the gap between the population mean and the individual patient, ultimately paving the way for safer and more effective personalized medicines.
Quantifying Variability: From Population PK to Machine Learning
Pharmacokinetics (PK), the study of how the body absorbs, distributes, metabolizes, and eliminates drugs, is fundamental to drug development and precision medicine. Two primary methodological approaches exist for conducting PK analysis: Individual PK and Population PK (PopPK). These approaches represent fundamentally different paradigms for understanding drug behavior. Individual PK focuses on deriving intensive concentration-time profiles and precise PK parameters for single subjects, typically through controlled studies with rich data collection [42] [43]. In contrast, Population PK studies variability in drug concentrations across a patient population using mathematical models, often from sparse, clinically realistic data, to identify and quantify sources of variability such as weight, age, or renal function [29] [44]. This analysis objectively compares these methodologies, framing the discussion within the broader scientific thesis of understanding population averages versus individual variation—a central challenge in pharmacological research and therapeutic individualization.
Core Methodological Differences
The distinction between Individual and Population PK extends beyond mere application to fundamental differences in data requirements, analytical frameworks, and underlying goals.
Foundational Principles and Data Requirements
- Individual PK often employs noncompartmental analysis (NCA), a model-independent approach that provides a direct description of the data, or compartmental analysis, which fits exponential equations to individual concentration-time data [42]. It requires rich, intensive sampling from each subject, with many samples collected at fixed intervals to fully characterize the drug's time-course [29] [44].
- Population PK uses nonlinear mixed-effects (NLME) modelling [45]. This approach simultaneously analyzes data from all individuals in a population. Its power lies in handling sparse data (only a few samples per patient) collected from unstructured dosing and sampling schedules, as is common in later-phase clinical trials or studies in vulnerable populations [29] [44].
Analytical Outputs and Interpretability
The outputs of these analyses also differ significantly, as summarized in Table 1.
- Individual PK Outputs: The primary results are specific PK parameters for each individual, such as maximum concentration (C~max~), area under the concentration-time curve (AUC), clearance (CL), and terminal half-life (t~1/2~) [42]. These are direct, intuitive measures of drug exposure.
- Population PK Outputs: The results include estimates of the typical (population average) value for each PK parameter (e.g., typical clearance), covariate effects (quantifying how patient characteristics like weight or renal function influence PK), and estimates of variability [29] [45]. This includes Between-Subject Variability (BSV) and Residual Unexplained Variability (RUV) [44]. This makes PopPK highly explanatory for variability but also more complex to interpret.
Table 1: Comparative Analysis of Individual vs. Population Pharmacokinetic Methods
| Feature | Individual PK | Population PK |
|---|---|---|
| Primary Focus | Intensive profile of a single subject | Variability in drug concentrations across a population [29] |
| Common Analysis Methods | Noncompartmental Analysis (NCA); One-/Two-compartment models [42] | Nonlinear Mixed-Effects (NLME) Modelling [45] |
| Data Requirements | Rich data (intensive sampling) [43] [44] | Sparse data (few samples per subject) acceptable [43] [44] |
| Handling of Covariates | Not directly integrated; requires subgroup analysis | Directly models effects of covariates (e.g., weight, age, renal function) [29] [44] |
| Key Outputs | C~max~, AUC, CL, V~d~, t~1/2~ for an individual [42] | Typical population parameters, covariate effects, estimates of variability (BSV, RUV) [45] [44] |
| Predictive & Simulative Utility | Limited to simulated profiles for a single, similar individual [42] | High; can simulate outcomes for diverse populations and novel dosing regimens [42] [43] |
| Primary Application Context | Early-phase clinical trials (Phase I), bioavailability/bioequivalence studies [42] [43] | Late-phase clinical trials (Phases II-IV), special populations, model-informed drug development (MIDD) [43] [29] |
Experimental Protocols and Data Analysis Workflows
Protocol for a Traditional Individual PK Study
A typical Individual PK study, such as a Phase I clinical pharmacology trial, follows a highly structured protocol.
- Study Design: A fixed-dose, parallel-group or crossover design is used. Subjects are healthy volunteers or carefully selected patients.
- Dosing and Sampling: A precise dose is administered, and blood samples are collected at pre-specified, frequent time points (e.g., pre-dose, 0.5, 1, 2, 4, 8, 12, 24 hours post-dose) to capture the complete concentration-time profile [29].
- Bioanalysis: Plasma or serum samples are analyzed using validated analytical methods (e.g., LC-MS/MS) to determine drug concentrations.
- Data Analysis:
- NCA: Concentrations are plotted against time. PK parameters are calculated directly using trapezoidal rule (for AUC), and observed C~max~ and t~max~ [42].
- Compartmental Analysis: Concentration-time data for each subject is fit to one-, two-, or three-compartment models using software like Phoenix WinNonlin. The model with the best statistical fit (e.g., lowest Akaike Information Criterion) is selected for each individual [42] [45].
Protocol for a Population PK Analysis
Population PK analysis is an iterative process of model development and evaluation, as outlined in the workflow below. It often uses pooled data from multiple studies [43] [44].
Diagram 1: Workflow for developing and evaluating a population pharmacokinetic model. (VPC: Visual Predictive Check; BSV: Between-Subject Variability; RUV: Residual Unexplained Variability)
The key steps involve:
- Data Assembly: Data from Phase 2/3 trials or therapeutic drug monitoring (TDM) is pooled. This includes drug concentrations, dosing histories, and patient covariates [44].
- Structural Model Development: A base PK model (e.g., one- or two-compartment) is built using NLME software (e.g., NONMEM, Monolix) to describe the typical concentration-time profile in the population [45] [46].
- Statistical Model Development: Inter-individual variability (IIV) and residual error (RUV) models are added to account for random variability not explained by the structural model [45] [44].
- Covariate Model Development: Covariates (e.g., body size, organ function) are tested for their influence on PK parameters to explain IIV. This is often done using stepwise forward addition/backward elimination, where a change in the objective function value (OFV) of >3.84 (p<0.05) for adding one parameter is considered statistically significant [45] [46].
- Model Evaluation: The final model is rigorously evaluated using goodness-of-fit plots, prediction-corrected visual predictive checks (pcVPC), and bootstrap methods [47] [45].
- Simulation: The qualified model is used to simulate drug exposure for various subpopulations and dosing scenarios to inform dosing recommendations [43] [44].
Supporting Experimental Data and Case Studies
Quantitative Evidence from Comparative Studies
Recent research provides quantitative data supporting the application and performance of these methods. A 2025 study by El Hassani et al. directly investigated the impact of sample size on PopPK model evaluation. Using a small real-world dataset from 13 elderly patients receiving piperacillin/tazobactam and a large virtual dataset of 1000 patients, they found that small clinical datasets produced consistent model evaluation results compared to large virtual datasets. Specifically, the bias and imprecision for the Hemmersbach-Miller model were -37.8% and 43.2% (population) for the clinical dataset, versus -28.4% and 40.2% for the simulated dataset, with no significant difference in prediction error distributions [47]. This validates that small, clinically sourced datasets can be robust for external PopPK model evaluation, a key advantage of the approach.
Another 2025 study compared a novel Scientific Machine Learning (SciML) approach with traditional PopPK and classical machine learning for predicting drug concentrations. The results, summarized in Table 2, show that the performance of methods can be context-dependent. For the drug 5FU, the MMPK-SciML approach provided more accurate predictions than traditional PopPK, whereas for sunitinib, PopPK was slightly more accurate [48]. This highlights that while new methods are emerging, PopPK remains a powerful and robust standard.
Table 2: Performance Comparison of PK Modeling Approaches from a 2025 Study [48]
| Drug | Modeling Approach | Performance Outcome |
|---|---|---|
| 5-Fluorouracil (5FU) | Population PK (PopPK) | Less accurate predictions than SciML |
| 5-Fluorouracil (5FU) | Scientific Machine Learning (MMPK-SciML) | More accurate predictions than PopPK |
| Sunitinib | Population PK (PopPK) | Slightly more accurate predictions than SciML |
| Sunitinib | Scientific Machine Learning (MMPK-SciML) | Slightly less accurate predictions than PopPK |
Application in Biosimilar Development
PopPK/PD modeling is critical in developing biologic drugs and biosimilars. A 2025 PopPK/PD analysis of the denosumab biosimilar SB16 used a two-compartment model with target-mediated drug disposition (TMDD) to characterize its PK profile. An indirect response model captured its effect on lumbar spine bone mineral density (BMD). The analysis conclusively showed that body weight accounted for 45% of the variability in drug exposure, but this translated to a clinically meaningless change of less than 2% in BMD [46]. Furthermore, the treatment group (SB16 vs. reference product) was not a significant covariate, successfully demonstrating biosimilarity and supporting regulatory approval. This case exemplifies how PopPK/PD moves beyond simple bioequivalence to build a comprehensive understanding of a drug's behavior.
The Scientist's Toolkit: Essential Reagents and Software
Successful execution of PK studies relies on a suite of specialized reagents and software solutions.
Table 3: Key Research Reagent Solutions and Software Tools
| Tool Category | Example Products/Assays | Function in PK Analysis |
|---|---|---|
| Bioanalytical Instruments | LC-MS/MS (Liquid Chromatography with Tandem Mass Spectrometry), ECLIA (Electrochemiluminescence Immunoassay) [46] | Quantification of drug and metabolite concentrations in biological matrices (e.g., plasma, serum) with high sensitivity and specificity. |
| Population PK Software | NONMEM [49], Monolix Suite [46], Phoenix NLME [42] | Industry-standard NLME modeling software for PopPK model development, estimation, and simulation. |
| Individual PK / NCA Software | Phoenix WinNonlin, R/Python packages | Performing noncompartmental analysis and individual compartmental model fitting. |
| Machine Learning & Automation Tools | pyDarwin [49] | Frameworks for automating PopPK model development using machine learning algorithms like Bayesian optimization. |
The choice between Individual and Population PK is not a matter of superiority but of strategic application, reflecting the necessary balance between understanding central tendencies and individual variations in pharmacology. Individual PK, with its intensive sampling and model-independent NCA, provides the definitive gold standard for characterizing a drug's baseline PK profile in highly controlled settings, making it indispensable for early-phase trials and bioequivalence studies [42]. Population PK, leveraging sparse data and powerful NLME modeling, excels at explaining variability and predicting outcomes in diverse, real-world populations, making it a cornerstone of late-stage drug development, precision dosing, and regulatory submission [43] [29] [44].
The evolution of the field points toward greater integration and automation. Emerging approaches like Scientific Machine Learning (SciML) show promise in enhancing predictive accuracy, sometimes surpassing traditional PopPK [48]. Furthermore, the automation of PopPK model development using frameworks like pyDarwin can drastically reduce manual effort and timelines while improving reproducibility [49]. For researchers and drug developers, a synergistic strategy that utilizes Individual PK for foundational profiling and Population PK for comprehensive characterization and simulation across the development lifecycle is paramount for efficiently delivering safe and effective personalized therapies.
Leveraging Sparse and Intensive Sampling Designs in Population PK Studies
In pharmacometrics, a fundamental tension exists between characterizing the population mean and understanding individual variation. This dichotomy directly influences the choice of pharmacokinetic (PK) sampling strategy. Intensive sampling designs, which collect numerous blood samples per subject, traditionally provide the gold standard for estimating PK parameters in individuals but are often impractical in clinical settings. In contrast, sparse sampling designs, which collect limited samples from each subject but across a larger population, leverage population modeling approaches to characterize both population means and inter-individual variability [50] [51]. The core challenge lies in determining how much information can be reliably extracted from sparse data without compromising parameter accuracy. Population modeling using non-linear mixed-effects (NLME) methods can disentangle population tendencies from individual-specific characteristics, making sparse sampling a viable approach for studying drugs in real-world patient populations where intensive sampling is ethically or logistically challenging [52]. This guide objectively compares these competing approaches, examining their performance, applications, and limitations within modern drug development.
Comparative Analysis of Sampling Design Performance
Quantitative Comparison of Key Performance Metrics
The table below summarizes a direct comparison of sparse versus intensive sampling based on experimental findings.
| Performance Metric | Sparse Sampling Design | Intensive Sampling Design |
|---|---|---|
| Typical Samples per Subject | 2-4 samples [50] | ≥7 samples [50] |
| Model Structure Identification | Reliable for complex (3-compartment) models [51] | Gold standard for model identification |
| Parameter Accuracy (vs. True Values) | Clinically acceptable accuracy for clearance and volume [50] [51] | High accuracy for individual parameters |
| Concentration Prediction Performance | Accurate prediction of concentrations after multiple doses [51] | Highly accurate individual concentration-time profiles |
| Primary Analysis Method | Population PK (NLME) with Bayesian priors [50] | Standard PK (NCA) or population PK |
| Key Requirement | Prior knowledge of drug PK in adults for stability [50] | No prior knowledge required |
| Logistical & Ethical Feasibility | High in special populations (pediatrics, critically ill) | Low in special populations |
Case Study Data: Morphine Pharmacokinetics
A post-hoc analysis of morphine PK in healthy volunteers demonstrated the robustness of sparse sampling. Using only 3 samples per subject (NPAG-3) versus 9 samples per subject (NPAG-9), the population model maintained predictive power [51]:
- Prediction Bias: The NPAG-3 model showed a minimal bias of +0.5 mg/L when predicting concentrations in a separate validation cohort receiving multiple boluses and infusions.
- Precision: The root mean squared error (RMSE) was 0.8 mg/L for the sparse sampling model, indicating clinically acceptable precision.
- Parameter Stability: Key parameters like plasma clearance (CL) remained stable at approximately 30 mL/kg/min across sampling intensities [51].
Experimental Protocols and Methodologies
Protocol for Sparse Sampling Population PK Analysis
The methodology for implementing a successful sparse sampling study, as validated in multiple analyses, involves a structured workflow.
Workflow for Sparse Sampling Analysis
Define Analysis Objectives and Prior Knowledge: The foundation of a robust sparse data analysis is the incorporation of prior knowledge of the drug's pharmacokinetics, typically from adult studies or rich data sources [50]. This serves as the initial parameter estimates for the structural model and informs the choice of prior distributions for Bayesian estimation.
Sparse Sampling Scheme Design: A sampling schedule is devised, typically collecting 2-4 blood samples per subject [50]. The timing can be fixed (all subjects sampled at identical times) or variable (different times per subject), with studies showing both can yield accurate estimates [50].
Data Collection and Population Model Development: Following data collection from a sufficiently large population, a base NLME model is developed. Software like NONMEM is conventionally used for this step [49] [52].
Parameter Estimation using Bayesian Methods: The core of the analysis involves post-hoc Bayesian estimation. This technique combines the sparse individual data with the previously established population model (the prior) to derive refined, individual-specific PK parameter estimates [50].
Model Validation: The final model must be validated. For the morphine case study, this involved predicting concentrations in a separate validation cohort that received multiple doses, assessing bias and precision [51].
Protocol for Intensive Sampling Analysis
The methodology for intensive sampling provides a reference point for comparison.
- Rich Data Collection: Each subject is intensively sampled, with ≥7 blood samples collected at strategic times post-dose to fully characterize the concentration-time curve [50].
- Individual and Population Modeling: Data can be analyzed via two primary pathways:
- Standard PK Analysis: PK parameters are estimated for each individual separately using non-compartmental analysis (NCA) or compartmental modeling. Population means and variances are then calculated from individual parameter estimates.
- Population PK Analysis: The rich data can also be analyzed using NLME modeling, which simultaneously estimates population and individual parameters. This approach is particularly valuable for quantifying inter-individual variability with high precision.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The table below details key computational tools and methodologies essential for executing the analyses described in this guide.
| Tool/Solution | Primary Function | Application Context |
|---|---|---|
| NONMEM | Industry-standard software for NLME modeling [49] [52] | Gold standard for population PK model development and parameter estimation |
| pyDarwin | Automated model search using machine learning (Bayesian optimization, genetic algorithms) [49] | Accelerates structural model development, especially for complex extravascular drugs |
| Automated Initial Estimate Pipeline (R package) | Data-driven generation of initial parameter estimates for PopPK models [53] | Crucial for automating modeling workflows and handling sparse data scenarios |
| Post-hoc Bayesian Estimation | Algorithm to derive individual PK parameters from sparse data using a population prior [50] | Core technique for individual parameter estimation in sparse sampling studies |
| NLME Framework | Statistical methodology to model fixed (population mean) and random (individual variation) effects simultaneously [52] | Foundational for all population PK analyses |
| Model Diagnostics (VPC, pcVPC) | Visual and numerical checks of model performance and predictive power [52] | Essential for qualifying a model as "fit-for-purpose" |
Emerging Trends and Automated Solutions
The field is rapidly evolving toward greater automation to reduce manual effort and improve reproducibility. Machine learning approaches are now being applied to automate the PopPK model development process. For instance, one framework using pyDarwin and a generic model search space was able to reliably identify model structures comparable to expert-developed models in less than 48 hours, evaluating fewer than 2.6% of the models in the search space [49]. Furthermore, automated pipelines for generating initial parameter estimates are being developed to handle both rich and sparse data, filling a critical gap in the modeling workflow [53]. These advances are particularly valuable for analyzing sparse data, where traditional methods like non-compartmental analysis (NCA) struggle [53].
Another emerging area is the automated extraction of prior knowledge from literature. Supervised classification pipelines have been developed that can identify tables containing in vivo PK parameters in scientific literature with high accuracy (F1 > 96%), paving the way for automated curation of large-scale PK databases to inform future studies [54]. The logical flow of these automated approaches is summarized in the following diagram.
Automated PK Analysis Workflow
The choice between sparse and intensive sampling designs is not a matter of superiority but of strategic alignment with research goals. The evidence demonstrates that sparse sampling, when coupled with robust population PK methodologies and prior knowledge, can yield population parameter estimates and predictive performance comparable to those derived from intensive sampling [50] [51]. The following strategic guidance is recommended:
- Use Intensive Sampling for Phase I studies, definitive model structure identification, and when studying drugs with complex or unknown PK profiles.
- Implement Sparse Sampling in late-phase clinical trials, pediatric studies, oncology, and other special populations where intensive sampling is not feasible. This approach is essential for characterizing the impact of patient-specific covariates on PK in the target population.
- Adopt Automated Tools like pyDarwin and initial estimate pipelines to accelerate model development, enhance reproducibility, and systematically explore model spaces that may be intractable with manual methods [49] [53].
The ongoing industrialization of pharmacometrics, through standardized reporting [52] and machine learning automation [49] [54], solidifies the role of sparse sampling as a powerful, validated approach for integrating population mean and individual variation research into efficient drug development.
The Power of Mixed-Effects and Multilevel Models to Partition Variance
In the ongoing scientific dialogue that pits population mean effects against individual variation, mixed-effects and multilevel models have emerged as a powerful methodological framework that bridges these perspectives. By explicitly partitioning variance into components attributable to systematic biological differences, contextual influences, and measurement error, these models provide a more nuanced understanding of complex biological and pharmacological phenomena. This guide objectively compares the performance of mixed-effects modeling approaches against traditional alternatives, demonstrating through experimental data their superior capability to handle hierarchical data structures, account for non-independence, and provide robust inference for both population-level trends and individual-specific variation—particularly valuable in drug development applications where both average treatment effects and between-subject variability critically inform dosing decisions and therapeutic personalization.
The fundamental tension between understanding population averages and individual differences represents a core challenge in biological and pharmacological research. Traditional statistical methods often focus exclusively on population mean effects, potentially obscuring important variation between individuals, experimental sites, or biological replicates. Mixed-effects models (also known as multilevel or hierarchical models) resolve this false dichotomy by simultaneously modeling population-level fixed effects and variance components at multiple hierarchical levels [55] [56].
These models recognize that biological data often possess inherent hierarchical structures—cells within patients, repeated measurements within subjects, or patients within clinical sites—where observations within the same cluster may be more similar to each other than to observations from different clusters. Ignoring this non-independence risks pseudoreplication and potentially inflated Type I error rates, where true effects are overstated or spurious effects are detected [55]. By explicitly modeling these variance components, mixed-effects approaches provide more accurate parameter estimates and appropriate uncertainty quantification.
In drug development particularly, understanding between-subject variability (BSV) is not merely a statistical nuisance but a substantive research interest. Population modeling approaches identify and describe relationships between subjects' physiologic characteristics and observed drug exposure or response, directly informing dosage recommendations to improve therapeutic safety and efficacy [28].
Fundamental Concepts: Variance Partitioning in Mixed-Effects Models
Fixed versus Random Effects
Mixed-effects models incorporate both fixed and random effects:
- Fixed effects represent systematic, reproducible influences or population-average relationships (e.g., experimental treatment conditions, demographic factors) where the levels of the factor are of specific interest and are not randomly sampled from a larger population [55] [57].
- Random effects account for variability introduced by hierarchical grouping structures or random sampling of units from a larger population (e.g., patients from multiple clinical sites, repeated measurements within individuals) [55].
The distinction often depends on the research question and study design. As Gelman & Hill (2007) note, "Absolute rules for how to classify something as a fixed or random effect generally are not useful because that decision can change depending on the goals of the analysis" [55].
Variance Partitioning Coefficients and Intraclass Correlation
The variance partitioning coefficient (VPC) and intraclass correlation coefficient (ICC) quantify how variance is apportioned across different levels of a hierarchy. In a simple two-level random intercept model, the ICC represents the proportion of total variance occurring between groups:
[ \rhoI = \frac{\sigma{u0}^2}{\sigma{u0}^2 + \sigma{e0}^2} ]
Where (\sigma{u0}^2) represents between-group variance and (\sigma{e0}^2) represents within-group variance [56].
For example, Gonzalez et al. (2012) investigated clustering of young adults' BMI within families, reporting a between-family variance ((\sigma{u0}^2)) of 8.92 and within-family variance ((\sigma{e0}^2)) of 13.92, yielding an ICC of 0.391—indicating that 39.1% of BMI variation occurred between families, while 60.9% occurred between young adults within families [56].
Table 1: Key Variance Partitioning Metrics
| Metric | Formula | Interpretation | Application Context |
|---|---|---|---|
| Intraclass Correlation (ICC) | (\rhoI = \frac{\sigma{u0}^2}{\sigma{u0}^2 + \sigma{e0}^2}) | Proportion of total variance due to between-group differences | Two-level hierarchical data |
| Variance Partition Coefficient (VPC) | (VPC = \frac{\sigma{level}^2}{\sigma{total}^2}) | Proportion of variance attributable to a specific level | Models with ≥3 levels or random slopes |
| Conditional VPC | (VPC = \frac{\sigma{u0}^2}{\sigma{u0}^2 + \sigma{e0}^2 + \sigma{fixed}^2}) | Variance proportion after accounting for fixed effects | Models with explanatory variables |
Workflow for Variance Partitioning Analysis
The following diagram illustrates the conceptual workflow for conducting variance partitioning analysis in complex biological studies:
Methodological Comparison: Mixed-Effects Models versus Traditional Approaches
Comparative Analysis of Modeling Approaches
Table 2: Comparison of Statistical Modeling Approaches for Hierarchical Data
| Approach | Key Characteristics | Variance Handling | Typical Applications | Limitations |
|---|---|---|---|---|
| Separate Models per Group | Fits independent model to each cluster | Ignores between-group information | Groups are fundamentally different (e.g., different species) | High variance with small group samples; no borrowing of information |
| Fixed Effects (Categorical) | Includes group indicator as fixed effect | Groups share common residual variance | All groups of interest are included; small number of groups | Incorrect SEs with group-level predictors; limited with many groups |
| Mixed-Effects Models | Includes group-specific random effects | Explicitly partitions within- and between-group variance | Clustered, longitudinal, or hierarchical data | Computational complexity; distributional assumptions |
| Naive Pooled Analysis | Pools all data ignoring group structure | Complete pooling; no group-level variance | Groups are functionally identical | Severe bias when groups differ |
| Two-Stage Approach | Fits individual models then combines estimates | Separate estimation then aggregation | Individual curve fitting with summary | Problems with sparse data; inefficient |
Experimental Evidence from Pharmacometric Applications
In drug development, the superiority of mixed-effects approaches is particularly evident. Early methods for population pharmacokinetic modeling included the "naive pooled approach" (fitting all data while ignoring individual differences) and the "two-stage approach" (fitting each individual separately then combining parameter estimates). Both methods exhibited significant problems with sparse data, missing samples, and other data deficiencies, resulting in biased parameter estimates [28].
The nonlinear mixed-effects (NLME) modeling framework introduced by Sheiner et al. addressed these limitations by allowing pooling of sparse data from many subjects to estimate population mean parameters, between-subject variability (BSV), and covariate effects that explain variability in drug exposure [28] [58]. This approach provides several advantages:
- Borrowing of information across all individuals improves accuracy of parameter estimates for any single individual
- Stable estimation even with sparse longitudinal data
- Explicit quantification of between-subject and within-subject variability
- Proper handling of missing data and variable measurement times
A 2019 study in Scientific Reports demonstrated the power of NLME modeling for in vitro drug response data using the Cancer Cell Line Encyclopedia (CCLE) and Genomics of Drug Sensitivity in Cancer (GDSC) datasets. The research identified consistently sensitive or resistant cancer cell lines by fitting NLME models to dose-response data, with CCL-specific random effects providing more stable estimates of drug response parameters through information borrowing across all cell lines [58].
Quantitative Results: Variance Partitioning in Practice
Case Study: Gene Expression Analysis with variancePartition
Hoffman and Schadt (2016) developed the variancePartition software to interpret drivers of variation in complex gene expression studies. Applying their method to four large-scale transcriptome profiling datasets revealed striking patterns of biological and technical variation that were reproducible across datasets [59].
Their linear mixed model framework partitions variation in each expression trait attributable to differences in disease status, sex, cell or tissue type, ancestry, genetic background, experimental stimulus, or technical variables. The model formulation:
[ y = \sum{j} X{j}\beta{j} + \sum{k} Z{k} \alpha{k} + \varepsilon ]
Where (Xj) are fixed effects matrices, (Zk) are random effects matrices, and variance components are estimated via maximum likelihood. The fraction of variation explained by each component is calculated as:
[ \text{Fraction}{component} = \hat{\sigma}^{2}{component} / \hat{\sigma}^{2}_{Total} ]
This approach accurately estimates variance fractions even for complex experimental designs where standard ANOVA is inadequate [59].
Case Study: Multilevel Analysis of Healthcare Data
In a multilevel analysis of in-hospital mortality among very low birthweight neonates in Bavaria, Esser et al. (2014) found a between-hospital variance ((\sigma_{u0}^2)) of 0.324 after adjusting for individual casemix. Using the latent variable method for multilevel logistic regression, the variance partition coefficient was calculated as:
[ VPC = \frac{0.324}{0.324 + 3.29} = 0.090 ]
This indicated that 9.0% of total variation in mortality was attributable to differences between hospitals after casemix adjustment, with the remaining 91.0% relating to differences between patients within hospitals [56].
Table 3: Variance Partitioning Examples Across Disciplines
| Research Domain | Variance Components | Key Findings | Data Source |
|---|---|---|---|
| Gene Expression Analysis | Tissue type (21.3%), Individual (15.6%), Sex (1.2%), Residual (61.9%) | Tissue type is primary driver of expression variation | variancePartition analysis [59] |
| Healthcare Outcomes | Between-hospital (9.0%), Within-hospital (91.0%) | Moderate hospital effect on neonatal mortality | Esser et al. (2014) [56] |
| Body Mass Index | Between-family (39.1%), Within-family (60.9%) | Substantial familial clustering of BMI | Gonzalez et al. (2012) [56] |
| Cancer Pharmacogenomics | Between-cell line, Within-cell line, Drug-specific | Identified consistently sensitive/resistant cell lines | Scientific Reports (2019) [58] |
Experimental Protocols and Methodologies
Protocol: Nonlinear Mixed-Effects Modeling for Dose-Response Data
The analysis of dose-response data in cancer cell lines exemplifies proper application of NLME modeling [58]:
Experimental Design:
- Data Source: Cancer Cell Line Encyclopedia (CCLE) - 24 compounds across 504 cancer cell lines
- Response Measurement: 8-point dose-response curves
- Model Selection: Compare 3-parameter vs. 4-parameter logistic models
Model Specification: For a given drug, let (y{ij}) represent the jth dose-response at (ni) drug doses for the ith cell line. The relationship is described by:
[ y{ij} = f(x{ij}, \betai) + e{ij} ]
Where (f(x{ij}, \betai)) is typically a 4-parameter logistic function:
[ f(x{ij}, \betai) = \beta{1i} + \frac{\beta{2i} - \beta{1i}}{1 + e^{[\beta{4i}(\log x{ij} - \beta{3i})]}} ]
Parameters (\beta{1i}) and (\beta{2i}) represent responses at infinite and zero concentrations, (\beta{3i}) is the relative EC50, and (\beta{4i}) is the Hills slope.
Estimation Procedure:
- Determine optimal functional form for each drug (3P vs. 4P logistic)
- Fit NLME model to drug-response data for each cancer type and drug combination
- Estimate cell-line specific random effects
- Identify outliers (consistently sensitive/resistant cell lines)
Protocol: Variance Partitioning in Multilevel Logistic Regression
For binary outcomes, variance partitioning requires special approaches as the standard linear mixed model assumptions don't apply [56]:
Latent Variable Approach:
- Assume the observed binary outcome (y{ij}) arises from an underlying continuous latent variable (y{ij}^*)
- Specify the model for the latent variable: [ y{ij}^* = \beta0 + \beta1 x{1ij} + \cdots + u{0j} + e{0ij}^* ]
- Substitute constant variance (\pi^2/3 \approx 3.29) for the lowest-level variance
- Calculate intraclass correlation: [ \rhoI = \frac{\sigma{u0}^2}{\sigma_{u0}^2 + \pi^2/3} ]
Simulation Method (Goldstein et al., 2002):
- Fit the multilevel logistic model
- Simulate values from the estimated model
- Calculate variance components from simulated data
- Compute variance partition coefficients
Application in Healthcare Research: Merlo et al. (2012) modeled probability of death using a 4-level model: individuals within households within census tracts within municipalities. They calculated cumulative variance partition coefficients as [56]:
[ VPCM = \frac{\sigmaM^2}{\sigmaM^2 + \sigmaC^2 + \sigma_H^2 + \pi^2/3} ]
[ VPCC = \frac{\sigmaM^2 + \sigmaC^2}{\sigmaM^2 + \sigmaC^2 + \sigmaH^2 + \pi^2/3} ]
[ VPCH = \frac{\sigmaM^2 + \sigmaC^2 + \sigmaH^2}{\sigmaM^2 + \sigmaC^2 + \sigma_H^2 + \pi^2/3} ]
The Scientist's Toolkit: Essential Research Reagents and Software
Computational Tools for Mixed-Effects Modeling
Table 4: Essential Software Tools for Mixed-Effects Modeling and Variance Partitioning
| Tool/Software | Primary Application | Key Features | Implementation |
|---|---|---|---|
| lme4 (R) | General linear mixed-effects models | Flexible formula specification; handles crossed and nested random effects | R statistical environment [55] |
| variancePartition (R) | Genome-wide variance partitioning | Quantifies contribution of multiple variables; parallel processing | Bioconductor package [59] |
| NLME | Nonlinear mixed-effects modeling | Pharmacokinetic/pharmacodynamic modeling; population PK/PD | R and S-PLUS [28] |
| Graphical Analysis | Visualization of variance components | ICC plots; variance decomposition diagrams | ggplot2, custom scripts [59] |
Experimental Design Considerations
Proper application of mixed-effects models requires careful experimental design:
Sample Size Planning:
- More variance at higher levels requires more clusters to achieve same power
- Design effect formula: (DEFF = 1 + (n - 1) \times ICC) where n is cluster size
- With high ICC, increasing individuals per cluster less efficient than adding clusters
Level Specification:
- Correctly identify all relevant hierarchical levels
- Omitted levels bias variance components for remaining levels
- Assume independence between clusters; account for spatial or temporal correlation if present
Centering Decisions:
- Grand mean centering for continuous variables when zero not meaningful
- Group mean centering when relative position within group is of interest
- Interpretation of intercepts depends on centering approach [60]
Mixed-effects and multilevel models provide an essential statistical framework for partitioning variance in complex biological and pharmacological data. By explicitly modeling hierarchical structures and quantifying variance components at multiple levels, these approaches enable researchers to move beyond simplistic population averages while avoiding the pitfalls of analyzing individual clusters separately. The methodology offers particular value in drug development contexts where understanding between-subject variability is crucial for therapeutic personalization.
Experimental evidence across diverse domains—from gene expression analysis to healthcare outcomes research and cancer pharmacogenomics—demonstrates that mixed-effects models consistently provide more accurate parameter estimates, appropriate handling of non-independent data, and richer biological insight than traditional approaches. As the complexity of biological datasets continues to grow, the ability to partition and interpret variance components will remain an essential skill for researchers seeking to understand both population trends and individual variation.
Utilizing N-of-1 and Replicated Crossover Trial Designs for Individual Response
For decades, the parallel-group randomized controlled trial (PG-RCT) has been the undisputed gold standard for establishing treatment efficacy, primarily answering the question: "What treatment works on average for a population?" [61]. However, this population-average focus often obscures a critical reality: individuals respond differently to treatments. The growing field of personalized medicine demands methods that can illuminate these individual response patterns, shifting the focus from "What works on average?" to "What works for this patient?" [32]. This paradigm has brought N-of-1 trials and replicated crossover designs to the forefront as powerful methodologies for directly measuring and understanding individual treatment responses, especially for chronic conditions with stable symptoms and short-acting interventions [62] [63].
N-of-1 trials are multi-period, double-blinded, controlled crossover experiments conducted within a single individual [64]. In these trials, a patient sequentially receives two or more interventions in a randomized order, often separated by washout periods to minimize carryover effects. A replicated crossover design typically refers to a study where a group of patients all undergo the same crossover sequence, and the data are analyzed primarily at the group level to estimate an average treatment effect. In contrast, a series of N-of-1 trials involves multiple patients each undergoing their own N-of-1 trial, with the focus first on individual-level analysis, though results can be aggregated to draw population inferences [65]. This guide provides a detailed comparison of these two powerful designs for investigating individual response.
Head-to-Head Comparison: Operational Characteristics
The following table summarizes the core design features, statistical properties, and ideal use cases for aggregated N-of-1 trials and traditional crossover designs based on simulation studies and methodological reviews.
Table 1: Comparison of N-of-1 and Crossover Trial Designs
| Characteristic | Aggregated N-of-1 Trials | Traditional Crossover Trials |
|---|---|---|
| Core Unit of Inference | Individual patient response, with potential for population aggregation [65] | Population-average treatment effect [65] |
| Typical Structure | Multiple cycles (e.g., AB/BA) per patient; designs can be individualized [64] [61] | Typically two periods (AB/BA) or variations (ABC, BCA) across a patient group [63] |
| Statistical Power & Sample Size | Higher power; requires far fewer patients than PG-RCTs to achieve the same power [62] [66] | Higher power than PG-RCTs; requires about half the participants of a parallel design [63] |
| Key Advantages | - Optimizes personalized clinical decisions- Estimates patient-level random effects- Flexible designs (e.g., open-label lead-in) can improve recruitment [62] [61] | - Each patient acts as their own control- Reduces between-subject variability- Detects smaller effect sizes with fewer subjects than parallel designs [63] |
| Key Challenges & Risks | - Higher Type I error with unaccounted carryover or selection bias- Risk of autocorrelation and missing data- Complex statistical analysis with no "gold standard" [62] [64] | - Susceptible to carryover and period effects- Unethical for curative treatments or severe, unstable conditions- Longer participant commitment increases dropout risk [63] [67] |
| Ideal Applications | - Chronic, stable conditions (e.g., ADHD, chronic pain)- Personalized medicine & biomarker validation- Ultra-rare genetic diseases [62] [68] [61] | - Symptomatic chronic conditions (e.g., migraines, hot flushes)- Short-lived, reversible treatment effects- Pharmacokinetic studies [63] [67] |
Quantitative Performance: Statistical Operating Characteristics
Simulation studies provide direct, quantitative comparisons of how these designs perform under controlled conditions. A 2019 simulation study that conducted 5000 simulated trials offers key insights into their statistical properties [62] [66].
Table 2: Statistical Operating Characteristics from Simulation Studies
| Performance Metric | Aggregated N-of-1 Trials | Crossover Trials | Parallel RCTs |
|---|---|---|---|
| Power (Probability of detecting a true effect) | Outperforms both crossover and parallel designs [62] [66] | Intermediate | Lowest |
| Sample Size (to achieve a given power) | Smallest required sample size [62] [66] | Intermediate | Largest required sample size |
| Type I Error (Probability of a false positive) | Higher than crossover and parallel designs when carryover effects or selection bias are not accounted for [62] [66] | Lower than N-of-1 designs when carryover is present [62] | Lower than N-of-1 designs when carryover is present [62] |
| Estimation of Patient-Level Effects | Allows for better estimation of patient-level random effects [62] [66] | Not designed for individual-level estimation | Not designed for individual-level estimation |
Experimental Protocols and Analytical Frameworks
Core Protocol for a Standard N-of-1 Trial
A typical N-of-1 trial is a multi-cycle, double-blinded experiment within a single patient. Each cycle consists of two periods where the patient is randomly assigned to receive either treatment A (e.g., active drug) or treatment B (e.g., placebo or control), with an untreated washout period between periods to mitigate carryover effects [64]. The fundamental workflow for a 3-cycle trial is illustrated below.
Figure 1: Workflow of a Multi-Cycle N-of-1 Trial
Advanced Design: An Aggregated N-of-1 Trial with Open-Label Lead-In
To address real-world challenges like recruiting acutely symptomatic patients, more complex aggregated N-of-1 designs have been developed. These may incorporate an initial open-label stabilization phase where all participants receive active treatment, followed by a series of blinded N-of-1 cycles [61]. This design was tested in a simulation study for a PTSD pharmacotherapy, prazosin, to evaluate its power for detecting a predictive biomarker. The study found that this hybrid design provided superior power over open-label or open-label with blinded discontinuation designs, and similar power to a traditional crossover design, while offering the clinical benefit of initial open-label treatment for all participants [61].
Analytical Approaches for N-of-1 Data
Analyzing data from N-of-1 trials presents unique challenges, including autocorrelation and the need to model within-subject variance. No single "gold standard" exists, but several statistical methods are commonly employed, each with strengths and weaknesses [64].
Table 3: Statistical Methods for Analyzing N-of-1 Trial Data
| Method | Description | Best Use Cases | Key Considerations |
|---|---|---|---|
| Paired t-test | Treats each cycle (A vs. B) as a pair and analyzes all pairs from all subjects [64]. | Preliminary analysis; simple, quick comparison. | Does not account for between-subject effects or autocorrelation; violates assumptions of independence [64]. |
| Mixed Effects Model of Difference | Models the within-cycle treatment difference (A-B) as the outcome, including random subject effects to account for the correlation of cycles within the same individual [64]. | Standard analysis for aggregated N-of-1 trials where the focus is on an overall treatment effect. | Accounts for between-subject heterogeneity. More robust than a simple t-test. |
| Mixed Effects Model (Full) | Models all raw outcome data, including fixed effects for treatment, period, and potential carryover effects, and random effects for subjects [64]. | Optimal when carryover or period effects are suspected and need to be explicitly modeled and estimated. | Most complex model but provides the most comprehensive assessment of design factors. |
| Meta-analysis | Treats each individual's trial as a separate study, calculates an effect size for each, and then pools them using a random-effects model [64]. | Combining results from a series of truly independent N-of-1 trials where individual-level estimates are of interest. | Not well-defined for a single N-of-1 trial (n=1). |
Successfully implementing these trial designs requires a suite of methodological tools and assessments.
Table 4: Essential Reagents and Resources for Trial Implementation
| Tool Category | Specific Examples | Critical Function |
|---|---|---|
| Statistical Software | R (with lmer function), SAS [62] [64] |
Fitting complex mixed-effects models to account for within-subject correlation and random effects. |
| Clinical Outcome Assessments (COAs) | Seizure logs, structured neurologic rating scales, wearable biometric sensors (e.g., for gait measurement) [68] | Quantifying disease-specific symptoms and treatment response; should be patient-centered and relevant to the genotype-phenotype. |
| Safety Monitoring Biomarkers | CSF sampling (cell count, protein), blood tests (liver function, platelets), urinalysis (proteinuria) [68] | Monitoring for potential toxicity, especially for novel therapeutic modalities like intrathecal ASOs. |
| Blinding & Randomization | Centralized randomization service, matched placebo [65] | Ensuring allocation concealment and minimizing bias in treatment assignment and outcome assessment. |
The choice between aggregated N-of-1 trials and replicated crossover designs is not a matter of one being universally superior. Instead, it is dictated by the primary research question. Crossover trials remain a powerful and efficient design for estimating the population-average treatment effect when individual response profiles are not the central interest [65]. In contrast, aggregated N-of-1 trials are uniquely equipped for the goals of personalized medicine, directly characterizing individual-specific treatment effects and validating predictive biomarkers, all while requiring fewer participants than traditional trials to achieve comparable power for population estimates [62] [61]. As medicine continues its march toward personalization, and with the recent advent of individualized genetic therapies that may be applicable to a single patient, the rigorous framework provided by N-of-1 trials will become increasingly indispensable for translating population data into optimal care for the individual [68].
Traditional statistical research has long relied on the concept of the population mean (µ), which represents the average value for an entire group, calculated as the sum of all values divided by the total number of elements in the population [69]. While this approach provides valuable insights into group-level characteristics, it inherently obscures individual variation—the unique patterns, behaviors, and outcomes that distinguish one person from another within the same population [69]. The limitations of population-level analysis become particularly pronounced in fields like healthcare and pharmaceutical development, where effective interventions must account for individual patient characteristics, genetic makeup, and environmental factors.
The emergence of big data, machine learning (ML), and artificial intelligence (AI) has fundamentally transformed our ability to model and predict individual outcomes. These technologies can analyze complex sequences of life events, medical histories, and behavioral patterns to generate personalized forecasts with remarkable accuracy [70] [71]. Predictive AI specifically utilizes statistical analysis and machine learning to identify patterns, anticipate behaviors, and forecast upcoming events by analyzing historical data and trends [72]. This capability represents a paradigm shift from population-centered modeling to individualized prediction, enabling more targeted interventions across numerous domains including healthcare, pharmaceutical development, and personalized medicine.
This guide provides a comprehensive comparison of emerging approaches in outcome prediction, examining their experimental protocols, performance metrics, and practical applications. By synthesizing current research and experimental data, we aim to equip researchers and drug development professionals with the knowledge needed to select and implement the most appropriate predictive modeling techniques for their specific requirements.
Comparative Analysis of Predictive Approaches
The table below summarizes the key characteristics, performance metrics, and optimal use cases for major categories of predictive modeling approaches, highlighting their applications in predicting individual outcomes.
Table 1: Comparison of Major Predictive Modeling Approaches for Individual Outcomes
| Approach | Core Methodology | Key Performance Metrics | Reported Performance | Primary Applications | Sample Size Requirements |
|---|---|---|---|---|---|
| Transformer-based Models (life2vec) | Analyzes life events as sequential data using transformer architecture [70] | Prediction accuracy, Model robustness [70] | Significantly outperforms state-of-the-art models for early mortality and personality prediction [70] | Early mortality prediction, Personality trait assessment, Life outcome forecasting [70] | Very large (e.g., 6 million individuals) [70] |
| Deep Learning with Sequential Medical Data | Processes sequential diagnosis codes using RNNs, LSTMs, or Transformers [73] | Area Under ROC (AUROC), Area Under Precision-Recall Curve (AUPRC) [73] | Positive correlation between training sample size and AUROC performance (P=.02) [73] | Next-visit diagnosis, Heart failure prediction, Mortality forecasting [73] | Large (performance improves with size) [73] |
| Traditional Machine Learning | Applies algorithms like regression, decision trees, SVMs to structured data [72] | Accuracy, Precision, Recall, F1-score [74] | Varies by algorithm and application; requires cross-validation for reliability [75] | Customer behavior prediction, Sales forecasting, Basic risk assessment [72] | Moderate (can work with smaller samples) [75] |
| Mathematical Modeling | Uses mechanistic models based on biological knowledge [76] | Model fit, Predictive accuracy [76] | Superior to AI when data is sparse; provides biological interpretability [76] | Cancer treatment response, Disease progression modeling [76] | Flexible (works with limited data) [76] |
| Hybrid AI-Mathematical Models | Combines AI training with mathematical model structure [76] | AUROC, Sensitivity, Specificity [76] | Potentially exceeds individual approach performance; enhances reproducibility [76] | Computational immunotherapy, Treatment optimization [76] | Large (for AI components) [76] |
Performance Considerations and Limitations
Each modeling approach demonstrates distinct strengths and limitations in handling the tension between population-level patterns and individual variations. Transformer-based models like life2vec show remarkable capability in capturing complex life course patterns but require exceptionally large datasets—the published model was trained on data from over six million individuals [70]. Similarly, deep learning models for healthcare predictions show a statistically significant positive correlation (P=.02) between training sample size and model performance as measured by AUROC [73].
For contexts with limited data, mathematical modeling provides an advantage because it incorporates existing biological knowledge rather than relying exclusively on data-driven pattern recognition [76]. These models are particularly valuable in novel treatment domains like immunotherapy, where sufficient clinical data may not yet be available for training robust AI models [76].
The integration of multiple data types consistently enhances predictive performance across approaches. In deep learning healthcare models, the inclusion of additional features such as medications (45% of studies), demographic data, and time intervals between visits generally correlated with improved predictive performance [73].
Experimental Protocols and Methodologies
Protocol 1: Transformer-based Life Sequence Modeling (life2vec)
The life2vec framework exemplifies the application of natural language processing techniques to human life sequences, representing a sophisticated approach to modeling individual variation within large populations [70].
Table 2: life2vec Experimental Protocol Components
| Protocol Phase | Key Components | Implementation Details | Outcome Measures |
|---|---|---|---|
| Data Collection | Danish national registry data [70] | Information on health, education, occupation, income, address with day-to-day resolution [70] | Comprehensive life sequences for 6 million individuals [70] |
| Data Representation | Life events as sequential tokens [70] | Each life event converted to a structured token, analogous to words in a sentence [70] | Continuous sequence representing individual life course [70] |
| Model Architecture | Transformer-based encoder [70] | Two-stage training: pre-training to learn structure, then fine-tuning for specific predictions [70] | Efficient vector representations of individual lives [70] |
| Prediction Tasks | Early mortality, Personality traits [70] | Classification of mortality risk (30-55 age group); Extraversion-Introversion prediction [70] | Probability scores for each outcome [70] |
| Validation | Performance comparison against baseline models [70] | Robustness checks for missing data; Evaluation across population segments [70] | Significant outperformance of state-of-the-art models [70] |
Protocol 2: Deep Learning for Sequential Medical Data
Healthcare prediction using sequential diagnosis codes requires specialized handling of temporal medical data with irregular intervals and complex coding structures [73].
Table 3: Deep Learning Healthcare Prediction Protocol
| Protocol Phase | Key Components | Implementation Details | Outcome Measures |
|---|---|---|---|
| Data Source | Electronic Health Records (EHRs) [73] | Structured EHRs with diagnosis codes, procedures, lab results [73] | Temporal patient records with visit sequences [73] |
| Data Preprocessing | Sequential diagnosis codes, Time intervals [73] | Conversion of medical codes to embeddings; Handling of irregular time intervals [73] | Visit sequences with embedded diagnoses [73] |
| Model Selection | RNN/LSTM (56%), Transformers (26%) [73] | Choice depends on data characteristics and prediction task [73] | Trained model for specific healthcare prediction [73] |
| Feature Integration | Multiple data types (45% include medications) [73] | Incorporation of demographics, medications, lab results [73] | Multi-feature input representation [73] |
| Validation Approach | Internal/external validation [73] | Split-sample validation; Few studies (8%) assess generalizability [73] | Performance metrics (AUROC, AUPRC) [73] |
Implementing predictive modeling approaches requires specific data, computational resources, and analytical tools. The following table details essential components for establishing a predictive analytics research pipeline.
Table 4: Essential Research Reagents and Resources for Predictive Modeling
| Resource Category | Specific Examples | Function/Role in Research | Implementation Considerations |
|---|---|---|---|
| Data Resources | National registries (e.g., Danish registers) [70] | Provide comprehensive population data for training models | Requires secure access; Ethical approval needed [70] |
| Data Resources | Electronic Health Records (EHRs) [73] | Source of sequential medical data for healthcare predictions | Must handle irregular time intervals; Privacy concerns [73] |
| Computational Frameworks | Transformer architectures [70] [73] | Process sequential data with attention mechanisms | Computationally intensive; Requires GPU resources [70] |
| Computational Frameworks | RNN/LSTM networks [73] | Model temporal sequences in healthcare data | Effective for regular sequences; May struggle with long gaps [73] |
| Validation Tools | Cross-validation methods (k-fold, LOOCV) [75] | Assess model performance and prevent overfitting | Essential for small datasets; Computational cost varies [75] |
| Validation Tools | PROBAST (Prediction Model Risk of Bias Tool) [73] | Standardized assessment of prediction model studies | Identifies methodological weaknesses in study design [73] |
| Interpretability Methods | Saliency maps [70] | Identify influential features in model predictions | Enhances trust and understanding of model decisions [70] |
| Interpretability Methods | Explainable AI (XAI) techniques [72] | Provide transparency in model decision-making | Critical for regulatory compliance and clinical adoption [72] |
The emerging approaches surveyed in this comparison guide demonstrate significant advances in predicting individual outcomes by leveraging big data, machine learning, and AI. While transformer-based models like life2vec show remarkable performance for life course predictions, and deep learning sequences excel in healthcare forecasting, the choice of approach must align with specific research constraints—particularly data availability and computational resources [70] [73].
A critical insight from current research is that hybrid approaches combining AI with mathematical modeling may offer superior performance, especially in data-sparse environments like novel drug development and immunotherapy [76]. Furthermore, the emphasis on explainability and generalizability continues to grow, with increasing recognition that predictive models must not only perform well but also provide interpretable results that can be trusted in high-stakes environments like healthcare and pharmaceutical development [70] [73].
As these technologies evolve, the tension between population-level patterns and individual variations will remain central to methodological development. Researchers and drug development professionals must carefully consider their specific use cases, data resources, and validation requirements when selecting and implementing these emerging approaches for predicting individual outcomes.
Overcoming Analytical Challenges in Variability Assessment
Identifying and Mitigating Unexplained Variability in Drug Exposure-Response
In pharmacological research and clinical practice, a fundamental tension exists between the population-oriented perspective of drug development and the individual-focused reality of patient care. Regulatory agencies and pharmaceutical companies primarily seek doses that are, on average, safe and effective for the patient population, leading to dosing recommendations most appropriate for a hypothetical "average patient" [32]. However, this population-based approach often fails to account for the profound interindividual heterogeneity in drug response observed in clinical settings, affecting both drug efficacy and toxicity [77]. This variability presents significant challenges, with studies indicating that only 50-75% of patients respond beneficially to the first drug offered for a wide range of diseases, while approximately 6.5% of hospital admissions are related to adverse drug reactions [77].
The recognition that individuals possess unique characteristics influencing drug disposition and response has catalyzed the emergence of precision medicine approaches. A compelling study conducted at the Mayo Clinic revealed that 99% of patients carried an actionable variant in at least one of five major pharmacogenomic genes, with only 1% having no actionable variants [32]. This genetic diversity, combined with non-genetic factors, creates substantial variability in systemic exposure following a fixed dose, often spanning 3 to 5-fold ranges and sometimes extending to 25-fold or more for specific medications [32]. This variability underscores the critical need to identify and mitigate unexplained variability in drug exposure-response relationships to optimize therapeutic outcomes for individual patients rather than population averages.
The Multifactorial Nature of Interindividual Variability
Drug response variability arises from a complex interplay of drug-specific, human body, and environmental factors operating across different biological organization levels [77]. The human body functions as a hierarchical, network-based system with multiple scales—molecular, genomic, epigenomic, transcriptomic, proteomic, metabolomic, cellular, tissue, organ, and whole-body—each contributing to the overall drug response phenotype [77]. Within and between these levels, molecules interlink to form biological networks whose properties, including robustness and redundancy, significantly influence drug effects.
The factors contributing to interindividual variability can be categorized as follows:
- Genetic factors: Variations influencing both pharmacokinetics (drug absorption, distribution, metabolism, elimination) and pharmacodynamics (therapeutic efficacy and adverse effects) [78]
- Demographic and physiological factors: Age-related changes in organ function, gender differences, body weight and composition [78]
- Disease states: Pathological conditions that alter drug metabolism and host responsiveness [78]
- Environmental and lifestyle factors: Diet, smoking, alcohol consumption, concurrent medications [78]
- Psychological factors: Individual variations in stress levels, psychological state, drug history, expectancy, and placebo responses [78]
This multifactorial complexity explains why pharmacogenomics, while valuable, has proven insufficient alone to adequately parse drug variability, necessitating more comprehensive approaches like systems pharmacology [77].
Quantitative Assessment of Variability: A Case Example
The extent of interindividual variability becomes particularly evident when examining specific medications. Research on atomoxetine in patients with attention-deficit/hyperactivity disorder (ADHD) demonstrates this phenomenon clearly [32]. When 23 pediatric patients aged 6-17 years were administered the recommended starting dose of 0.5 mg/kg, the resulting plasma concentration profiles revealed striking variability: a 25-fold range of concentrations at 4 hours and a remarkable 2,000-fold range at 24 hours post-administration [32].
Knowledge of CYP2D6 genotype, the primary clearance pathway for atomoxetine, explains some of this variability, as illustrated in Figure 1C [32]. However, considerable interindividual variability persists even within genotype groups, highlighting the limitations of single-gene approaches and the contribution of additional genetic and non-genetic factors to the observed variability in drug exposure [32].
Table 1: Factors Contributing to Interindividual Variability in Drug Response
| Factor Category | Specific Factors | Impact on Drug Response |
|---|---|---|
| Genetic | Polymorphisms in drug-metabolizing enzymes (e.g., CYP450 family), drug transporters, drug targets | Altered drug clearance, bioavailability, and target engagement |
| Physiological | Age, organ function, body composition, pregnancy | Changes in drug absorption, distribution, metabolism, excretion |
| Pathological | Renal/hepatic impairment, inflammation, disease severity | Modified drug disposition and target organ sensitivity |
| Environmental | Drug interactions, diet, smoking, environmental toxins | Enzyme induction/inhibition, altered protein binding |
| Treatment-related | Adherence, dosage regimen, drug formulation | Variable drug exposure over time |
Methodological Approaches for Identifying Unexplained Variability
Pharmacometric Modeling Strategies
Population pharmacokinetic (PopPK) approaches represent a fundamental methodology for identifying and quantifying sources of variability in drug concentration within patient populations [29]. Unlike traditional pharmacokinetic studies that involve multiple samples from small numbers of healthy volunteers, PopPK utilizes opportunistic samples collected from actual patients taking a drug under clinical conditions [29]. This approach employs non-linear mixed-effects modeling (NONMEM) to distinguish between fixed effects (population typical values) and random effects (interindividual and residual variability) [29] [38].
The PopPK modeling process involves:
- Developing a structural model describing drug absorption, distribution, and elimination
- Identifying covariates (patient characteristics) that systematically influence pharmacokinetic parameters
- Quantifying random effects including interindividual variability, inter-occasion variability, and residual unexplained variability [29] [38]
This methodology is particularly valuable for studying patient groups difficult to enroll in traditional trials, such as premature infants, critically ill patients, or those with organ impairment [29].
Exposure-response (E-R) modeling extends this approach by linking drug exposure metrics to pharmacological effects [79]. The relationship between drug exposure (typically area under the concentration-time curve or AUC) and treatment effect is quantitatively evaluated to establish the therapeutic window and identify factors contributing to variability in drug response [79] [38].
Advanced Integrative Approaches
Systems pharmacology has emerged as an interdisciplinary field that incorporates but extends beyond pharmacogenomics to parse interindividual drug variability [77]. This holistic approach to pharmacology systematically investigates all of a drug's clinically relevant activities in the human body to explain, simulate, and predict clinical drug response [77]. Systems pharmacology encompasses two complementary research themes:
- Pharmacologically-oriented systems biology: Utilizes high-throughput omics technologies to identify factors associated with differential drug response across biological hierarchy levels
- Pharmacometrics: Develops quantitative mathematical models describing a drug's pharmacokinetic and pharmacodynamic properties [77]
Model-Informed Drug Development (MIDD) represents another advanced framework that integrates quantitative approaches throughout drug development [80]. MIDD employs various modeling methodologies, including quantitative structure-activity relationship (QSAR), physiologically based pharmacokinetic (PBPK) modeling, semi-mechanistic PK/PD models, population PK/exposure-response (PPK/ER) analysis, and quantitative systems pharmacology (QSP) [80]. These approaches provide data-driven insights that accelerate hypothesis testing, improve candidate selection, and reduce late-stage failures.
Figure 1: Experimental Workflow for Identifying and Mitigating Unexplained Variability in Drug Exposure-Response
Experimental Protocols for Variability Assessment
Population Pharmacokinetic Study Design
Objective: To identify and quantify sources of variability in drug exposure in the target patient population.
Methodology:
- Patient Recruitment: Enroll patients representing the spectrum of the target population, including variability in age, organ function, concomitant medications, and other relevant characteristics [29]
- Sample Collection: Collect sparse blood samples (typically 2-4 samples per patient) at unpredictable times relative to dosing, reflecting real-world clinical practice [29]
- Drug Concentration Measurement: Utilize validated bioanalytical methods (e.g., UPLC-MS/MS) to quantify drug and metabolite concentrations in biological samples [79]
- Covariate Data Collection: Document potential sources of variability including demographic, physiological, laboratory, genetic, and treatment-related factors [29]
- Model Development: Employ non-linear mixed-effects modeling software (e.g., NONMEM) to:
- Model Validation: Evaluate model performance using goodness-of-fit plots, visual predictive checks, and bootstrap methods [79]
Key Considerations: Population PK studies are particularly valuable when traditional intensive sampling designs are impractical or unethical, such as in pediatric, geriatric, or critically ill populations [29].
Exposure-Response Modeling Protocol
Objective: To characterize the relationship between drug exposure and pharmacological response, accounting for sources of variability.
Methodology (based on kukoamine B case study [79]):
- Clinical Data Collection: Obtain data from placebo-controlled clinical trials, including drug concentrations, dosing records, and efficacy biomarkers (e.g., SOFA score for sepsis)
- Exposure Assessment: Calculate exposure metrics (e.g., AUC) using non-compartmental analysis or model-based approaches
- Response Modeling: Develop mathematical models linking exposure to response using non-linear mixed-effects modeling approaches:
- For continuous responses: Employ direct, indirect, or more complex response models
- For categorical responses: Utilize logistic or time-to-event models
- Covariate Analysis: Identify patient factors influencing the exposure-response relationship
- Model Evaluation: Assess model adequacy through diagnostic plots, visual predictive checks, and comparison of objective function values
- Simulation: Conduct model-based simulations to explore different dosing scenarios and optimize dosing strategies
Application Example: In the development of kukoamine B for sepsis, exposure-response modeling differentiated the drug effect from standard care therapy using a latent-variable approach combined with an inhibitory indirect response model, enabling dose optimization for phase IIb trials [79].
Table 2: Comparison of Methodologies for Assessing Variability in Drug Exposure-Response
| Methodology | Key Features | Data Requirements | Applications | Limitations |
|---|---|---|---|---|
| Population PK | Mixed-effects modeling, sparse sampling | 2-4 samples per patient, covariate data | Identifying sources of PK variability, dose individualization | Cannot directly assess efficacy outcomes |
| Exposure-Response | Links exposure metrics to clinical effects | Drug concentrations, efficacy measures | Dose optimization, identifying therapeutic window | Requires adequate range of exposures and responses |
| Systems Pharmacology | Integrates multi-scale biological data | Multi-omics data, PK/PD measurements | Comprehensive understanding of drug actions, biomarker discovery | Computational complexity, data integration challenges |
| Model-Informed Drug Development | Quantitative framework across development | Preclinical, clinical, and real-world data | Candidate selection, trial design, regulatory decision-making | Requires specialized expertise, model validation challenges |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Computational Tools for Variability Assessment
| Tool/Reagent | Category | Function | Example Applications |
|---|---|---|---|
| UPLC-MS/MS Systems | Analytical Instrumentation | Quantification of drug and metabolite concentrations in biological samples | Bioanalytical method validation, therapeutic drug monitoring [79] |
| Next-Generation Sequencing Platforms | Genomic Analysis | Identification of genetic variants influencing drug metabolism and response | Pharmacogenomic testing, discovery of novel variants [77] [32] |
| NONMEM Software | Computational Tool | Non-linear mixed-effects modeling for population PK/PD analysis | Population model development, covariate analysis [79] [81] |
| R/Python with Pharmacometric Packages | Statistical Programming | Data processing, visualization, and model diagnostics | Exploratory data analysis, diagnostic plotting, model evaluation [79] |
| PBPK Modeling Software | Simulation Platform | Mechanistic prediction of drug disposition based on physiology | Predicting drug-drug interactions, special population dosing [80] |
| Validated Biomarker Assays | Diagnostic Tools | Quantification of disease activity and therapeutic response | Exposure-response modeling, dose optimization [79] |
Comparative Analysis of Variability Mitigation Strategies
Quantitative Comparison of Methodological Performance
Table 4: Performance Comparison of Variability Mitigation Approaches
| Mitigation Strategy | Unexplained Variability Reduction | Implementation Complexity | Evidence Level | Clinical Impact |
|---|---|---|---|---|
| Therapeutic Drug Monitoring | 30-60% for specific drugs | Moderate | Multiple RCTs | High for narrow therapeutic index drugs |
| Pharmacogenomic Guidance | 20-50% for specific gene-drug pairs | Low to Moderate | Guidelines for >100 drugs | Moderate, limited to specific drug-gene interactions |
| Population PK Model-Informed Dosing | 25-45% across multiple drug classes | High | Population studies, some RCTs | Moderate to High, applicable broadly |
| Systems Pharmacology Approaches | 35-55% in research settings | Very High | Early research, case studies | Potentially High, still emerging |
| Machine Learning/AI Methods | 30-50% in research settings | High | Early research, limited validation | Potentially High, requires further validation |
Case Study: Kukoamine B Development for Sepsis
The development of kukoamine B for sepsis provides a compelling case study in exposure-response modeling to address variability and optimize dosing [79]. Researchers utilized data from a phase IIa clinical trial involving 34 sepsis patients to develop an exposure-response model linking kukoamine B exposure (AUC) to changes in SOFA score, a biomarker of organ dysfunction in sepsis [79].
Key findings and approaches included:
- Model Structure: A latent-variable approach combined with an inhibitory indirect response model effectively differentiated drug effects from standard care therapy
- Parameter Estimation: The maximum fraction of standard care therapy effect was estimated at 0.792, while the AUC at half maximal drug effect (EAUC50) was 1,320 h·ng/mL
- Dose Optimization: Model-based simulations demonstrated that SOFA scores on day 7 decreased to a plateau when AUC reached 1,500 h·ng/mL, supporting the selection of a 0.24 mg/kg dose for phase IIb trials [79]
This case exemplifies how quantitative modeling of exposure-response relationships, accounting for both drug and non-drug effects, can inform dosing decisions despite substantial interindividual variability.
The tension between population means and individual variation represents both a challenge and opportunity in clinical pharmacology. While population approaches provide the necessary foundation for drug development and initial dosing recommendations, they prove insufficient for optimizing therapy for individual patients, the majority of whom deviate from the population average in clinically relevant ways [32]. The future of effective pharmacotherapy lies in integrating population-level knowledge with individual-specific data through advanced pharmacometric approaches, systems pharmacology, and emerging technologies like artificial intelligence and machine learning [80] [32].
The most promising path forward involves collecting more comprehensive data—genomic, metabolomic, proteomic, clinical—from diverse populations and applying sophisticated analytical methods to identify patterns predictive of individual drug response [32]. This approach aligns with the emerging paradigm of precision medicine, where treatments are tailored to an individual's unique characteristics to optimize therapeutic outcomes while minimizing adverse effects [77] [78]. As these methodologies continue to evolve and validate in prospective clinical trials, they hold the potential to transform drug development and clinical practice, ultimately ensuring that no patient feels they are "just average" [32].
The pursuit of scientific discovery often relies on summarizing complex data into actionable insights. However, a fundamental tension exists between the convenience of population-level averages and the reality of individual variation. This is starkly illustrated by Simpson's Paradox, a statistical phenomenon where a trend appears in several different groups of data but disappears or reverses when these groups are combined [82]. In the field of drug development, where understanding variability in patient responses is critical, failing to account for this paradox can lead to profoundly incorrect conclusions about a treatment's efficacy and safety, ultimately directing research and resources down the wrong path.
What is Simpson's Paradox?
Simpson's Paradox occurs when the apparent relationship between two variables changes upon dividing the data into subgroups, typically due to a confounding variable or lurking variable that is not evenly distributed across groups [83] [84]. This is not just a mathematical curiosity; it is a common and problematic issue in observational data that underscores the dangers of relying solely on aggregated statistics without considering underlying strata.
At its core, the paradox reveals that statistical associations in raw data can be dangerously misleading if important confounding variables are ignored [85]. The reversal happens because the combined data does not account for the different sizes or base rates of the subgroups, improperly weighting the results [82] [84].
A Classic Example: Kidney Stone Treatment
A real-life example from a medical study compares the success rates of two treatments for kidney stones. The data reveals the paradoxical conclusion that Treatment A was more effective for both small and large stones, yet Treatment B appeared more effective overall [82].
Table: Success Rates for Kidney Stone Treatments
| Stone Size | Treatment A | Treatment B |
|---|---|---|
| Small Stones | 93% (81/87) | 87% (234/270) |
| Large Stones | 73% (192/263) | 69% (55/80) |
| Both (Aggregated) | 78% (273/350) | 83% (289/350) |
The paradox arose because the "lurking variable"—the size of the kidney stones—had a strong effect on the success rate. Doctors were more likely to assign the severe cases (large stones) to the perceived better treatment (A), and the easier cases (small stones) to Treatment B [82]. Consequently, the overall totals were dominated by the large number of easy cases in Treatment B (Group 2) and the difficult cases in Treatment A (Group 3), which skewed the aggregated results.
Simpson's Paradox in Drug Development and Research
The implications of Simpson's Paradox are particularly significant in clinical pharmacology and drug development, where the core mission is to understand and manage sources of variability in drug response [86]. The established paradigm of developing a drug based on an average effect observed in a population cohort can mask critical subgroup effects.
The Population Approach vs. Individual Variation
Drug development has traditionally been based on establishing a recommended dose that is tolerable and efficacious for a population average [87] [86]. This approach, often termed the "population approach" in pharmacokinetics, seeks to understand the typical drug profile while characterizing the sources and magnitude of variability within the population [87].
However, this model clashes with the goal of precision medicine, which aims to match the right drug and dose to the right patient. A drug dose deemed "safe and effective" on a population average could be ineffective for one genetic subgroup and toxic for another. This individual variation can be due to intrinsic factors like genetics, age, and gender, or extrinsic factors like diet and cultural practices [86].
Table: Factors Causing Population Diversity in Drug Responses
| Category | Examples of Factors | Impact on Drug Response |
|---|---|---|
| Intrinsic Factors | Genetics, Age, Gender, Body Size, Ancestry | Altered drug metabolism (PK), drug target sensitivity (PD), and risk of toxicity. |
| Extrinsic Factors | Diet, Concomitant Medications, Cultural Practices | Changes in drug absorption, metabolism, or overall exposure. |
Pharmacogenetics: A Key to Resolving the Paradox
Genetic variation is a major contributor to the phenotypic differences in drug response that can lead to Simpson-like reversals. A critical reason for ethnic or racial variability in drug response arises from different allelic frequencies of polymorphic drug-metabolising enzyme (DME) genes [86].
Case Study: 6-Mercaptopurine (6MP) 6MP is a drug used to treat acute lymphoblastic leukaemia. Its inactivation is governed by the enzyme thiopurine methyltransferase (TPMT). The TPMT gene is polymorphic, and patients homozygous for non-functional TPMT alleles can develop severe myelosuppression from standard doses [86]. While the non-functional TPMT*3A allele is more common in Caucasian populations (~5%), it is rare in East Asians. However, East Asian patients were still observed to be more susceptible to 6MP toxicity. This prompted further research, which uncovered polymorphisms in another gene, NUDT15, as the major genetic cause of this susceptibility in East Asian populations [86]. This example shows how an apparent population-level effect (increased toxicity in a subgroup) can be misunderstood without stratifying by the correct genetic confounding variable.
The Scientist's Toolkit: Navigating the Paradox
To avoid the pitfalls of Simpson's Paradox and correctly interpret data, researchers must employ specific methodologies and tools.
Key Research Reagent Solutions
Table: Essential Reagents and Resources for Pharmacogenetic Research
| Reagent/Resource | Function | Example/Application |
|---|---|---|
| DNA Sequencers | Identify genetic variants (SNPs, haplotypes) in candidate genes. | Discovering variant alleles in DMEs like TPMT and NUDT15 [86]. |
| Biobanks | Repository of well-characterized patient samples (DNA, tissue). | Correlating drug response phenotypes with genotypes from diverse populations [88]. |
| Pharmacogenetic Databases | Centralized resource for polymorphic variant data. | The Pharmacogenetic Polymorphic Variants Resource to lookup allele frequencies [88]. |
| Population PK/PD Software | Model drug kinetics and dynamics while accounting for variability. | NONMEM software for population pharmacokinetic analysis [87]. |
Experimental Protocols for Stratified Analysis
Protocol 1: Identifying Confounding through Causal Diagrams (DAGs)
- Define Variables: Identify the key variables: the intervention (e.g., drug treatment) and the outcome (e.g., recovery).
- Map Relationships: Construct a Directed Acyclic Graph (DAG) to hypothesize relationships. Include all potential common causes of the intervention and the outcome (confounders), such as disease severity, genetics, or demographic factors [85].
- Analyze Stratified Data: Collect data and analyze the intervention-outcome relationship within each level of the identified confounding variable (e.g., within each genetic subgroup). If the relationship is consistent and positive in all strata, it is more robust than the aggregated result.
Protocol 2: A/B Testing with Controlled Traffic Splits In clinical trial design or analysis, inconsistent allocation of participants can introduce a Simpson-like effect.
- Randomized Allocation: Ensure patients are randomly assigned to treatment groups to evenly distribute known and unknown confounders.
- Consistent Protocol: Maintain consistent allocation ratios and eligibility criteria throughout the study period. Changing the protocol mid-study can create imbalanced subgroups [89].
- Stratified Analysis Plan: Pre-specify subgroup analyses based on known biologically relevant factors (e.g., genotype, disease stage) to be examined alongside the primary aggregate analysis.
A Framework for Diagnosis and Resolution
The following workflow provides a structured, visual guide for researchers to diagnose and resolve Simpson's Paradox in their data.
Diagnosing Simpson's Paradox
Once diagnosed, the appropriate methodological approach must be selected to find the true causal effect.
Resolving Simpson's Paradox
Key Takeaways for Researchers
For researchers, scientists, and drug development professionals, navigating Simpson's Paradox is essential for robust and translatable findings.
- Always Stratify Data: Before drawing conclusions from aggregated data, investigate trends within relevant subgroups defined by potential confounders such as disease severity, genetic markers, or demographic factors [83] [85].
- Focus on Causal Inference: Move beyond statistical association. Use causal diagrams (DAGs) to model relationships and identify confounders. Employ methods like the do-calculus to estimate the effect of interventions more reliably [84] [85].
- Embrace Population Diversity: In drug development, proactively include diverse populations in early-phase trials. Use genetic and other biomarker data to stratify responses rather than relying on broad categories like race or ethnicity, which are social constructs and poor proxies for biological variation [86].
- Question the Average: The population mean can be a misleading guide for individual patient care. Understanding the distribution and sources of individual variation is the cornerstone of precision medicine and protects against the pitfalls of Simpson's Paradox.
Addressing Irreversible Conditions and Throughput Limits in Single-Subject Designs
In the landscape of scientific research, a fundamental tension exists between understanding population-level effects and accounting for individual variation. While group experimental designs traditionally focus on analyzing aggregate data through measures like the mean, this approach can mask critical individual differences and heterogeneous treatment responses [90]. Single-subject experimental designs (SSEDs) represent a powerful methodological alternative that prioritizes the intensive study of individual participants, serving as both their own control and unit of analysis [91] [92]. These designs are characterized by repeated measurements, active manipulation of independent variables, and visual analysis of data patterns to establish causal relationships at the individual level [93] [92].
However, SSEDs face two significant methodological challenges when applied to irreversible conditions and contexts requiring higher throughput. Irreversible conditions—where behaviors, learning, or treatment effects cannot be voluntarily reversed—create constraints for certain SSEDs that rely on withdrawal of treatment to demonstrate experimental control [92]. Simultaneously, throughput limits inherent in the intensive, repeated measurement requirements of SSEDs present practical challenges for research programs requiring larger participant numbers [91] [90]. This guide examines how researchers can address these challenges while maintaining methodological rigor within the broader context of understanding both individual variation and population-level effects.
Core Principles of Single-Subject Experimental Designs
Defining Characteristics and Methodological Foundations
Single-subject research involves studying a small number of participants (typically 2-10) intensively, with a focus on understanding objective behavior through experimental manipulation and control, collecting highly structured data, and analyzing those data quantitatively [91]. The defining features include: the individual case serving as both the unit of intervention and unit of data analysis; the case providing its own control for comparison; and the outcome variable being measured repeatedly within and across different conditions or levels of the independent variable [92].
SSEDs should not be confused with case studies or other non-experimental designs. Unlike qualitative case studies, SSEDs employ systematic manipulation of variables, controlled conditions, and quantitative analysis to establish causal inference [91] [92]. The key assumption underlying these designs is that discovering causal relationships requires manipulation of an independent variable, careful measurement of a dependent variable, and control of extraneous variables [91].
Phases, Measurement, and Visual Analysis
Single-subject designs are typically described according to the arrangement of baseline and treatment phases, often assigned letters such as A (baseline/no-treatment phase) and B (treatment phase) [92]. The baseline phase establishes a benchmark against which the individual's behavior in subsequent conditions can be compared, with ideal baseline data displaying stability (limited variability) and a lack of clear trend of improvement [93]. By convention, a minimum of three baseline data points are required to establish dependent measure stability, with more being preferable [93].
Analysis of experimental control in SSEDs relies primarily on visual inspection of graphed data, examining changes across three parameters: level (average performance), trend (slope of data), and variability [93]. When changes in these parameters are large and immediate following intervention, visual inspection is relatively straightforward. However, in more ambiguous real-life data sets, effects must be replicated within the study to rule out extraneous variables—a primary characteristic that provides internal validity to SSEDs [93].
Figure 1: Fundamental Workflow of Single-Subject Experimental Designs
The Irreversible Condition Challenge: Methodological Solutions
Understanding the Problem with Traditional Withdrawal Designs
The challenge of irreversible conditions emerges most prominently in traditional A-B-A withdrawal designs, which involve measuring behavior during baseline (A), implementing treatment during intervention (B), and then withdrawing treatment to return to baseline conditions (A) [92] [94]. This design requires the behavior to return to baseline levels during the second A phase to demonstrate experimental control. As noted in the research, "It's a hard behavior to implement in our field because we want our behaviors to stay up! We don't want to see them return back to baseline" [92].
The problem is particularly acute in educational, therapeutic, and medical contexts where treatments produce lasting learning, physiological changes, or skill acquisition that cannot or should not be reversed for ethical or practical reasons [92]. In these situations, traditional withdrawal designs become methodologically inappropriate and ethically questionable, requiring alternative approaches that can demonstrate experimental control without treatment withdrawal.
Design Solutions for Irreversible Conditions
Researchers have developed several robust SSED alternatives that circumvent the need for reversal while maintaining experimental rigor:
Table 1: Single-Subject Designs for Irreversible Conditions
| Design Type | Key Methodology | Experimental Control Mechanism | Best Applications |
|---|---|---|---|
| Multiple Baseline | Staggered introduction of intervention across behaviors, settings, or participants [94] | Demonstration that change occurs only when intervention is applied to each unit | Speech therapy, educational interventions, skill acquisition |
| Changing Criterion | Intervention phase divided into subphases with progressively more difficult performance criteria [95] | Behavior changes to match each new criterion level while maintaining stability | Habit formation, progressive skill building, tolerance development |
| Multiple Probe | Combination of multiple baseline with intermittent (probe) measurements to reduce testing fatigue [95] | Limited measurement with staggered intervention introduction | Complex skill sequences, behaviors susceptible to testing effects |
| B-A-B Design | Begins with intervention, withdraws to establish baseline, then reinstates intervention [94] | Ethical approach when initial baseline is impractical or unethical | Severe behaviors requiring immediate intervention |
Figure 2: Decision Pathway for Addressing Irreversible Conditions in Single-Subject Designs
The multiple baseline design is particularly valuable for addressing irreversible conditions as it demonstrates experimental control through the staggered introduction of treatment across different behaviors, settings, or participants [94]. This design requires that changes occur only when, and not until, the intervention is applied to each specific unit, effectively ruling out coincidental extraneous variables as explanations for observed effects. The key to proper implementation involves selecting functionally independent behaviors, settings, or participants and ensuring that baseline data collection continues for all units until treatment is sequentially introduced [94].
Throughput Limitations: Balancing Depth and Efficiency
Understanding Throughput Constraints in Single-Subject Research
The throughput limitations of SSEDs stem from their fundamental methodological requirements: intensive repeated measurements, extended baseline stabilization, and systematic replication across participants [93] [91]. While group designs can study large numbers of participants simultaneously, examining behavior primarily in terms of group means and standard deviations, single-subject research typically involves somewhere between two and ten participants studied in detail over time [91]. This creates practical constraints in research contexts requiring larger sample sizes, such as clinical trials, drug development, and educational program evaluation.
The throughput challenge is further compounded by the need for continuous data collection rather than single pre-test/post-test measurements [92]. As noted in methodological guidance, "Single-case experimental designs require ongoing data collection. There's this misperception that one baseline data point is enough. But for single-case experimental design you want to see at least three data points, because it allows you to see a trend in the data" [92]. This requirement, while methodologically essential, creates significant practical constraints on researcher time and resources.
Strategies for Optimizing Research Efficiency
Table 2: Addressing Throughput Limitations in Single-Subject Research
| Challenge | Traditional Approach | Efficiency Optimization Strategy | Methodological Safeguards |
|---|---|---|---|
| Participant Numbers | 1-10 participants typical [91] | Systematic replication protocols across labs | Clear operational definitions for independent/dependent variables |
| Measurement Intensity | Continuous measurement throughout all phases [92] | Technology-assisted data collection; multiple probe designs | Maintain minimum 3-5 data points per phase; ensure measurement fidelity |
| Baseline Duration | Continued until stability demonstrated [93] | Predetermined baseline length with validation checks | Statistical process control charts for stability determination |
| Analysis Complexity | Primarily visual analysis [93] | Complementary statistical methods; effect size measures | Training in visual analysis; consensus coding; blinded analysis |
| Generalization | Direct and systematic replication [90] | Hybrid designs combining single-subject and group elements | Planned replication series; detailed participant characterization |
Despite these throughput challenges, SSEDs offer countervailing efficiencies in early-stage intervention development. Their flexibility allows researchers to "understand what an individual does" before scaling up to larger trials, potentially avoiding costly failures in subsequent group studies [92]. This makes them particularly valuable in the context of drug development and behavioral treatment testing, where they can identify promising interventions and optimal implementation parameters before committing to large-scale randomized controlled trials (RCTs) [93] [90].
Complementary Methodological Approaches: Integrating Individual and Population Perspectives
The Complementary Roles of Single-Subject and Group Designs
Rather than viewing SSEDs and group designs as competing methodologies, contemporary research emphasizes their complementary relationship in building comprehensive evidence bases [93] [90]. Group designs (including between-group and within-subject comparisons) excel at characterizing effects across populations and analyzing combined effects of multiple variables, while single-subject designs provide more finely-focused internal validity by using the same subject as both experimental and control [90]. This complementary relationship enables researchers to address different types of research questions throughout the intervention development process.
The integration of these approaches is particularly valuable in evidence-based practice, where SSEDs can be implemented "prior to implementing a randomized controlled trial to get a better handle on the magnitude of the effects, the workings of the active ingredients" and then again "after you have implemented the randomized controlled trial, and then you want to implement the intervention in a more naturalistic setting" [92]. This sequential utilization of methodologies leverages the respective strengths of each approach while mitigating their individual limitations.
Hybrid and Sequential Methodological Applications
Advanced research programs increasingly employ multi-methodological approaches that combine single-subject and group methodologies to address complex research questions [90]. These hybrid approaches recognize that scientific rigor "does not proceed only from the single study; replication, systematic replication, and convergent evidence may proceed from a progression of methods" [90]. In practical terms, this might involve using SSEDs in early therapy development to establish proof of concept, followed by small-scale group studies to identify moderating variables, and culminating in large-scale RCTs to establish efficacy across populations.
This integrated approach is particularly valuable for addressing the complementary challenges of internal and external validity. While single-subject designs provide strong internal validity for the individuals studied, group designs (when properly implemented with appropriate sampling) can provide information about population-level generality [90]. The sequential application of both methodologies creates a more comprehensive evidence base than either approach could provide independently.
Experimental Protocols for Addressing Methodological Challenges
Protocol for Multiple Baseline Design (Addressing Irreversible Conditions):
- Select 3-5 functionally independent behaviors, settings, or participants
- Simultaneously begin continuous baseline measurement for all units
- Establish stability criteria (e.g., 3-5 consecutive data points with limited variability and no counter-therapeutic trend)
- Implement intervention for the first unit while continuing baseline measurement for others
- Sequentially introduce intervention to subsequent units only after demonstrating effect in previous unit
- Maintain intervention for each unit once introduced
- Analyze data for experimental control evidenced by changes occurring only when intervention is applied to each specific unit [94]
Protocol for Optimized Throughput in Clinical Settings:
- Implement technology-assisted data collection (e.g., automated recording, mobile applications)
- Establish clear operational definitions for both dependent and independent variables
- Train multiple observers to acceptable reliability standards (e.g., >80% interobserver agreement)
- Use multiple probe designs to reduce measurement burden when appropriate
- Plan for systematic replication across participants with varying characteristics
- Implement partial-intervention time series to assess component effectiveness [92] [95]
Essential Research Reagent Solutions
Table 3: Key Methodological Components for Rigorous Single-Subject Research
| Research Component | Function & Purpose | Implementation Considerations |
|---|---|---|
| Operational Definitions | Precisely define target behaviors and interventions in measurable terms | Must be objective, clear, and complete enough for replication |
| Stability Criteria | Establish predetermined standards for phase changes | Typically based on trend, level, and variability metrics across 3-5 data points |
| Social Validity Measures | Assess practical and clinical importance of effects | Should include stakeholder perspectives; treatment acceptability; quality of life impacts |
| Fidelity Protocols | Ensure consistent implementation of independent variable | Includes training materials, checklists, and periodic verification |
| Visual Analysis Guidelines | Standardize interpretation of graphed data | Should address level, trend, variability, immediacy of effect, and overlap |
| Systematic Replication Framework | Plan for extending findings across participants, settings, and behaviors | Sequential introduction of variations to establish generality boundaries |
The methodological challenges posed by irreversible conditions and throughput limitations in single-subject designs are significant but not insurmountable. Through appropriate design selection, implementation of multiple baseline and changing criterion approaches, and strategic integration with group methodologies, researchers can effectively address these constraints while maintaining scientific rigor. The complementary relationship between single-subject and group designs offers a powerful framework for understanding both individual variation and population-level effects, ultimately strengthening the evidence base for interventions across medical, educational, and psychological domains.
As research methodology continues to evolve, the strategic application of single-subject designs—with particular attention to their appropriate use for irreversible conditions and efficient implementation despite throughput constraints—will remain essential for developing effective, individualized interventions that account for the meaningful heterogeneity of treatment response across diverse populations.
Optimizing Study Power and Design to Detect Clinically Relevant Interactions
A fundamental tension exists in clinical research between identifying average treatment effects for a population and accounting for individual variation in treatment response. This challenge becomes particularly acute in the study of drug-drug interactions (DDIs), where a therapy's safety and efficacy can be dramatically altered by concomitant medications. The complexity of detecting these interactions is magnified by the rise of polypharmacy, especially among vulnerable populations such as cancer patients and the elderly [96] [97]. Traditionally, clinical trials have been powered to detect main effects—the population mean response to a single therapeutic agent. However, this approach often fails to capture the nuanced interindividual variation in drug response that arises from complex interactions, potentially overlooking clinically significant safety issues or efficacy failures.
The statistical and methodological frameworks used to investigate these phenomena are therefore critical. Research objectives must be clearly defined: are we seeking to understand the average interaction effect across a patient population, or are we trying to characterize the variation in interactions among individuals? This distinction shapes every aspect of study design, from sample size calculation to statistical analysis and clinical interpretation [98]. As treatment regimens grow more complex, optimizing study power and design to detect clinically relevant interactions is no longer a specialized concern but a fundamental requirement for patient safety and therapeutic success.
Statistical Foundations: Population Means Versus Individual Variation
Conceptual Framework
In clinical pharmacology, the concepts of "within-population" and "among-population" variation provide a crucial framework for designing interaction studies [99]. Within-population variation refers to the variability in drug response observed among individuals within a defined group (e.g., patients taking the same drug combination). This variation can arise from genetic polymorphisms, environmental factors, comorbidities, or other concomitant medications. In contrast, among-population variation describes systematic differences in average drug response between distinct groups (e.g., between different demographic groups or patient populations). Understanding and quantifying these sources of variation is essential for determining whether an observed interaction has consistent effects across a population or manifests differently in subpopulations [98].
The statistical definition of interaction itself is scale-dependent, leading to potentially different conclusions about clinical relevance based on the analytical approach [98]. On an additive scale, interaction is defined by risk differences: (r11−r01) ≠ (r10−r00), where r11 represents the risk in individuals exposed to both drugs, r01 represents risk with the first drug alone, r10 represents risk with the second drug alone, and r00 represents baseline risk with neither drug. On a multiplicative scale, interaction is defined by risk ratios: (r11/r01) ≠ (r10/r00). These different scales can lead to substantively different conclusions about the presence and magnitude of interactions, with the additive scale often being more relevant for clinical and public health decisions [98].
Implications for Study Design
The choice between these statistical models has direct implications for study power and design. Studies powered to detect interactions on a multiplicative scale may miss clinically important interactions that are evident on an additive scale, particularly when baseline risks differ among subpopulations [98]. This was illustrated in a study of Factor V Leiden, oral contraceptives, and deep vein thrombosis risk, where a multiplicative model found no interaction, while an additive model revealed an important three-fold increase in risk beyond what would be expected from the individual effects [98].
Table 1: Comparison of Interaction Measurement Scales
| Scale Type | Interaction Definition | Clinical Interpretation | Power Considerations |
|---|---|---|---|
| Additive | (r11−r01) ≠ (r10−r00) | Absolute risk difference; directly informs number needed to harm | Requires larger sample sizes for same effect size |
| Multiplicative | RR11 ≠ RR10 × RR01 | Relative risk ratio; familiar to clinicians from odds ratios | May miss interactions where absolute risk matters most |
| Sufficient-Component Cause | Co-participation in causal mechanism | Biological interaction; identifies synergistic pathways | Difficult to power without precise biological knowledge |
Methodological Approaches for Detecting Interactions
Conventional Versus Exposure-Response Powering
Traditional approaches to powering clinical studies for interaction detection rely heavily on comparing discrete patient groups. For a binary endpoint, conventional power calculations test the hypothesis H0:P1=P2 versus Ha:P1≠P2, where P1 and P2 are response probabilities in different dose groups [100]. The power calculation depends on the type I error rate (α), sample size (n), and the assumed effect size (P1−P2). This between-group comparison approach effectively measures among-population variation but may fail to capture the continuous relationship between drug exposure and response.
A more powerful exposure-response methodology leverages within-population variation in drug exposure to improve detection capabilities [100]. Rather than comparing groups, this approach tests whether the slope (β1) of the exposure-response relationship differs significantly from zero (H0:β1=0 vs Ha:β1≠0). This method incorporates pharmacokinetic data from phase I studies, particularly the distribution of drug exposures (e.g., AUC) in the population at a given dose, which follows log-normal distribution due to variability in drug clearance [100]. By modeling the continuous relationship between individual drug exposure and response, this approach can detect more subtle interactions and achieve equivalent power with smaller sample sizes.
Table 2: Power Comparison Between Conventional and Exposure-Response Methods
| Design Factor | Conventional Method | Exposure-Response Method |
|---|---|---|
| Hypothesis Test | H0:P1=P2 vs Ha:P1≠P2 | H0:β1=0 vs Ha:β1≠0 |
| Primary Endpoint | Binary response | Continuous or binary via logistic transformation |
| Key Input Parameters | Sample size, α, P1, P2 | Sample size, α, β0, β1, exposure distribution |
| PK Variability Consideration | Not directly incorporated | Directly incorporated via exposure distribution |
| Typical Sample Size | Larger for equivalent power | Smaller for equivalent power |
| Information Utilization | Between-group differences | Within-group and between-group variation |
Experimental Designs for Interaction Studies
The pharmacokinetic cross-over design is particularly efficient for studying drug-drug interactions [101]. In this design, each participant serves as their own control, receiving the investigational drug alone in one period and in combination with the interacting drug in another period. This within-subject comparison reduces variability by controlling for interindividual variation in drug metabolism and response, thereby increasing statistical power to detect interactions. The design is especially valuable for drugs with high between-subject variability in pharmacokinetics, as it effectively isolates the interaction effect from other sources of variation.
Key considerations for cross-over designs include appropriate washout periods to prevent carryover effects, log-transformation of pharmacokinetic parameters (AUC, Cmax) which typically follow log-normal distributions, and careful sample size calculations that account for within-subject correlation [101]. This design differs significantly from parallel group designs, which are more affected by among-population variation and typically require larger sample sizes to achieve equivalent power for detecting interaction effects.
Diagram 1: Cross-over design workflow for pharmacokinetic drug interaction studies. This efficient design controls for interindividual variation by having each participant serve as their own control [101].
Optimizing Power Through Exposure-Response Methodology
Implementation Framework
The exposure-response powering methodology follows a specific algorithmic approach that can be implemented through simulation [100]. This process begins with defining the exposure-response relationship, typically through a logistic regression model for binary endpoints: P(AUC)=1/(1+e^-(β0+β1·AUC)). The intercept (β0) and slope (β1) are calculated based on known response probabilities at specific exposures: β1 = (logit(P2)-logit(P1))/(AUC2-AUC1) and β0 = logit(P1)-β1·AUC1 [100].
The power calculation algorithm involves: (1) simulating n·m drug exposures from the known population distribution of clearance; (2) calculating probability of response for each simulated exposure using the logistic model; (3) simulating binary responses based on these probabilities; (4) performing exposure-response analysis on the simulated dataset; (5) determining significance at α=0.05; and (6) repeating this process for multiple study replicates (e.g., 1,000) to estimate power as the proportion of replicates with statistically significant exposure-response relationships [100]. This simulation-based approach allows researchers to explore various design parameters and their impact on statistical power before conducting actual studies.
Factors Influencing Power in Exposure-Response Analyses
Multiple factors impact the power of exposure-response analyses using logistic regression models [100]:
- Slope of exposure-response relationship: Steeper slopes (higher β1 values) generally increase power, as the effect becomes more detectable against background variation.
- Intercept value: The baseline response probability in the absence of drug (placebo effect) influences power, with extremely high or low baseline probabilities reducing power for detecting drug effects.
- Number of dose levels: Increasing from two to three doses typically enhances power by providing more information about the exposure-response shape.
- Dose range: Wider dose ranges improve power by increasing the leverage to estimate the exposure-response slope.
- PK variability: Higher coefficients of variation in drug exposure (e.g., 40% vs 25%) generally reduce power by increasing noise in the exposure-response relationship.
These factors interact in complex ways, making simulation-based power analysis particularly valuable for optimizing study designs for specific research contexts and anticipated effect sizes.
Diagram 2: Exposure-response power calculation algorithm. This simulation-based approach incorporates population pharmacokinetic variability to determine study power [100].
Reference Standards and Clinical Relevance
Establishing Reference Sets for DDI Detection
The development of reliable reference sets is crucial for validating methodologies to detect drug-drug interactions. The CRESCENDDI (Clinically-relevant REference Set CENtered around Drug-Drug Interactions) dataset addresses this need by providing 10,286 positive and 4,544 negative controls, covering 454 drugs and 179 adverse events mapped to standardized RxNorm and MedDRA terminology [96]. This resource enables systematic evaluation of signal detection algorithms by providing a common benchmark that reflects clinically relevant interactions rather than merely theoretical pharmacological effects.
The process for developing such reference sets involves extracting information from multiple clinical resources (e.g., British National Formulary, Micromedex), mapping drug names to standard terminologies, manual annotation of interaction descriptions to MedDRA concepts, and generating negative controls through systematic literature review [96]. This comprehensive approach helps distinguish true adverse drug interactions from background noise and coincidental associations, addressing the challenge that predicted DDIs based on pharmacological knowledge far outnumber those with clinically significant consequences.
Assessing Clinical Relevance
Not all statistically significant interactions are clinically relevant. Factors determining clinical relevance include the severity of the potential adverse outcome, the magnitude of the interaction effect, the therapeutic window of the affected drug, the availability of monitoring strategies or alternatives, and the patient population at risk [97]. For drugs with narrow therapeutic indices, such as many anticancer agents, even modest interactions can have serious clinical consequences, warranting more sensitive detection methods and lower thresholds for significance [97].
Methodological guidance from organizations such as the Italian Association of Medical Oncology (AIOM) and the Italian Society of Pharmacology (SIF) emphasizes structured frameworks for DDI risk assessment, management, and communication in clinical practice [97]. These frameworks help translate statistical findings into actionable clinical guidance, ensuring that research on interaction detection ultimately improves patient outcomes.
Table 3: Essential Research Reagents and Resources for DDI Studies
| Resource Category | Specific Examples | Function and Application |
|---|---|---|
| In Vitro Systems | Human liver microsomes, Cryopreserved hepatocytes, Recombinant enzymes | Screening for metabolic interactions; determining inhibition potential |
| Analytical Instruments | LC-MS/MS systems, HPLC with UV/fluorescence detection | Quantifying drug concentrations in biological matrices for PK studies |
| Reference Sets | CRESCENDDI, OMOP reference set | Benchmarking and validating signal detection algorithms |
| Clinical Databases | FDA Adverse Event Reporting System (FAERS), Electronic health records | Post-marketing surveillance and signal detection |
| Statistical Software | R, SAS, NONMEM, Phoenix WinNonlin | Power calculation, data analysis, pharmacokinetic modeling |
| Terminology Standards | MedDRA, RxNorm, WHO Drug Dictionary | Standardizing adverse event and drug coding across studies |
Optimizing study power and design to detect clinically relevant interactions requires thoughtful integration of multiple methodological approaches. The tension between population means and individual variation can be addressed through study designs that efficiently capture both within-subject and between-subject sources of variability. Exposure-response methods offer superior power compared to conventional group comparisons by leveraging continuous exposure data and incorporating population pharmacokinetic variability [100]. Cross-over designs further enhance power by controlling for interindividual variation [101]. As polypharmacy continues to increase, particularly in vulnerable populations, these methodological advances become increasingly essential for ensuring drug safety and efficacy in real-world clinical practice.
Future directions in interaction research include greater incorporation of genetic variability in drug metabolism, development of more sophisticated in silico prediction models, and integration of real-world evidence from electronic health records with traditional clinical trial data [102] [96]. By continuing to refine methodological approaches and validation frameworks, researchers can better detect and characterize clinically relevant interactions, ultimately improving patient care and treatment outcomes.
Strategies for Integrating Covariates to Reduce Residual Unexplained Variability
In the ongoing research of population means versus individual variation, a central challenge is distinguishing the true signal of a treatment effect from the noise of natural heterogeneity. Residual unexplained variability (RUV) refers to the variance in outcomes that remains after accounting for known sources of variation. Effectively integrating covariates to reduce this RUV is paramount for obtaining precise and powerful estimates in scientific studies, from clinical drug development to online controlled experiments. This guide compares established and emerging covariate adjustment techniques, evaluating their performance, methodological requirements, and suitability for different research contexts.
Understanding Covariate Adjustment Techniques
Covariate adjustment techniques use auxiliary data—patient characteristics, pre-experiment measurements, or other predictors—to explain a portion of the outcome variance that would otherwise be deemed random noise. This process sharpens the precision of the central parameter of interest, be it a population average treatment effect or an estimate of individual response.
The following table summarizes the core characteristics of key methods discussed in the literature.
Table 1: Comparison of Key Covariate Adjustment Techniques
| Technique | Core Principle | Key Advantages | Key Limitations | Best Suited For |
|---|---|---|---|---|
| Multivariate Regression (ANCOVA) [103] [104] | Regresses outcome on treatment indicator and baseline covariates. | Simple implementation; asymptotically unbiased if covariates are independent of treatment [103]. | Risk of bias if covariates are affected by the treatment; limited by linearity assumption [103]. | Standard RCTs with a few, pre-specified, continuous covariates. |
| CUPED [103] | Uses the pre-experiment mean of the outcome as a covariate in a linear model. | Simple, can be implemented without complex libraries; reduces variance unbiasedly [103]. | Limited to pre-experiment outcome data, cannot leverage other informative covariates [103]. | A/B tests and experiments with stable pre-period outcome data. |
| CUPAC [103] | Uses predictions from a machine learning model trained on pre-experiment data as the covariate. | Can capture non-linear relationships, potentially offering greater variance reduction than CUPED [103]. | Complex fitting/training; risk of bias if model uses features affected by the treatment [103]. | Scenarios with rich pre-experiment data and complex, non-linear covariate relationships. |
| Doubly Robust (DR) [103] [104] | Combines outcome regression and propensity score weighting. | Remains consistent for the ATE if either the outcome or propensity model is correct [103]. | Computationally complex, requires fitting multiple models [103]. | Studies where model misspecification is a major concern. |
| Overlap Weighting (OW) [104] | A propensity score-based method that weights subjects based on their probability of being in either treatment group. | Bounded weights, robust performance in high-dimensional settings, achieves excellent covariate balance [104]. | Targets the Average Treatment Effect on the Overlap (ATO), which is similar but not identical to the ATE in non-RCT settings [104]. | RCTs and non-randomized studies, especially with covariate imbalance or high-dimensional data [104]. |
Experimental Performance and Data
The theoretical advantages of these methods are validated by their performance in simulation studies and real-world applications. The choice of method can significantly impact the efficiency and reliability of the estimated effect.
Table 2: Comparative Performance of Adjustment Methods
| Method | Variance Reduction vs. Unadjusted | Impact on Statistical Power | Relative Bias | Key Findings from Studies |
|---|---|---|---|---|
| Unadjusted ANOVA | Baseline (0%) | Baseline | Low [104] | Unbiased by randomization but often inefficient [104]. |
| ANCOVA | Substantial (depends on ( R^2 )) [103] | Increased | Low [104] | Asymptotically guarantees variance reduction; performance hinges on correct linear specification [103] [104]. |
| CUPED | Substantial, similar to ANCOVA [103] | Increased | Low | A particular case of ANCOVA; effective and simple for pre-experiment outcomes [103]. |
| CUPAC | Can exceed CUPED with good predictors [103] | Increased | Low | Superior when the relationship between covariates and outcome is non-linear [103]. |
| Doubly Robust | Highest potential (theoretically optimal) [103] | Highest Potential | Low [104] | Achieves the lowest asymptotic variance in its class; robust to model misspecification [103] [104]. |
| Overlap Weighting (OW) | High, outperforms IPW and ANCOVA in simulations [104] | High | Low [104] | Found to have smaller RMSE and be more robust with high-dimensional covariates compared to other methods [104]. |
A practical application from Instacart demonstrated the power of these techniques. The company reported that using covariate adjustment for a key metric led to a median 66% reduction in variance, which directly translated to running experiments 66% faster for the same statistical power [105].
Furthermore, a 2024 simulation study comparing six methods found that Overlap Weighting performed best overall, exhibiting smaller root mean square errors (RMSE) and model-based standard errors, which resulted in higher statistical power to detect a true effect [104]. The study also highlighted that all methods can suffer from the "high-dimensional curse," where having too many covariates relative to sample size degrades performance, underscoring the need for careful variable selection [104].
Detailed Experimental Protocols
To ensure reproducibility and proper implementation, below are detailed protocols for two key approaches: a foundational regression-based method and a more advanced machine-learning-driven technique.
Protocol 1: Implementing CUPED (Controlled-experiment Using Pre-Experiment Data)
CUPED is a widely adopted method for variance reduction in randomized experiments [103].
- Pre-Experiment Data Collection: For each experimental unit (e.g., a user, patient, or subject), collect one or more historical measurements of the outcome variable (Y) from a period before the experiment began. Let X be this pre-experiment value.
- Randomization and Experimentation: Conduct the randomized experiment as usual, assigning units to treatment (T=1) and control (T=0) groups. Measure the outcome variable (Y) during the experiment.
- Calculate the Theta (θ) Parameter: Compute the parameter θ as the ratio of the covariance between the experimental outcome (Y) and the pre-experiment covariate (X) to the variance of X. This is equivalent to the slope of a linear regression of Y on X. ( \theta = \frac{{\text{cov}(Y, X)}}{{\text{var}(X)}} ) This can be done on the entire dataset or separately for each treatment arm.
- Create an Adjusted Outcome: For each unit, calculate an adjusted outcome ( Y{\text{adj}} ): ( Y{\text{adj}} = Y - \theta \cdot (X - \muX) ) where ( \muX ) is the overall mean of the pre-experiment covariate X.
- Estimate the Treatment Effect: The Average Treatment Effect (ATE) is calculated as the difference in means of the adjusted outcome ( Y{\text{adj}} ) between the treatment and control groups. ( \tau{\text{CUPED}} = \bar{Y}{\text{adj,T}} - \bar{Y}{\text{adj,C}} ) This estimator is unbiased and has lower variance than the simple difference-in-means [103].
Protocol 2: Implementing a Novel Pre- and In-Experiment Data Combination
Recent research introduces methods that go beyond pre-experiment data to achieve greater variance reduction [106].
- Data Collection:
- Pre-Experiment Covariates ((X{\text{pre}})): Gather baseline characteristics (e.g., user demographics, historical activity).
- In-Experiment Covariates ((X{\text{in}})): Identify and collect data on variables that are measured during the experiment and are highly correlated with the final outcome but are not themselves outcomes of the treatment (e.g., early engagement signals in a long-term study).
- Model Training (Pre-Experiment):
- Use a machine learning model (e.g., LightGBM, linear regression) trained only on control group data from a pre-experiment period. The model predicts the outcome Y using (X{\text{pre}}).
- Let ( g(X{\text{pre}}) ) be the predicted outcome from this model. This serves as a sophisticated covariate similar to CUPAC.
- Model Training (In-Experiment):
- Similarly, train a separate machine learning model on control group data from the experiment period. This model predicts the outcome Y using the in-experiment covariates (X{\text{in}}).
- Let ( h(X{\text{in}}) ) be the prediction from this model.
- Regression Adjustment:
- Fit a linear regression model on the experimental data where the experimental outcome Y is regressed on:
- The treatment indicator (T)
- The pre-experiment prediction ( g(X{\text{pre}}) )
- The in-experiment prediction ( h(X{\text{in}}) )
- The coefficient of the treatment indicator T in this regression is the estimated ATE, adjusted for both pre- and in-experiment information.
- Fit a linear regression model on the experimental data where the experimental outcome Y is regressed on:
- Validation: This method maintains unbiasedness because the covariates are constructed from models trained solely on control group data or use pre-experiment data, ensuring they are independent of the treatment assignment [106]. Applied at Etsy, this method with only a few in-experiment covariates yielded substantial variance reduction beyond CUPAC [106].
Methodological Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for selecting and applying a covariate adjustment strategy, integrating concerns for both population-level inference and individual variation.
The Scientist's Toolkit: Essential Reagents and Solutions
Successfully implementing these strategies requires both conceptual knowledge and practical tools. The table below details key "research reagents" for a modern covariate analysis.
Table 3: Essential Reagents for Covariate Integration Experiments
| Tool/Reagent | Function/Purpose | Example Use Case |
|---|---|---|
| Pre-Experiment Data | Serves as a baseline covariate to explain between-subject variability; must be independent of treatment [103] [106]. | User's historical conversion rate (CUPED), pre-trial biomarker measurements. |
| In-Experiment Data | Covariates measured during the trial that are strongly correlated with the final outcome but not consequences of treatment [106]. | Early user engagement metrics, intermediate physiological measurements. |
| Body Size/Composition Metrics | Standard, mechanistically plausible covariates for pharmacokinetic parameters (Clearance, Volume) [107] [108]. | Allometric scaling of body weight for dose individualization. |
| Organ Function Markers | Explain predictable variability in drug elimination and exposure [107]. | Creatinine Clearance (CLcr) for renal function, albumin for hepatic function. |
| Propensity Score Model | Estimates the probability of treatment assignment given covariates; used in weighting methods like OW and AIPW [104]. | Creating balanced groups in observational studies or improving efficiency in RCTs. |
| Machine Learning Model (e.g., LightGBM) | Used in CUPAC and DR estimation to create powerful predictive covariates from complex, non-linear data [103]. | Generating a predicted outcome based on a large set of pre-experiment features. |
| Consistent Variance Estimator | Calculates accurate standard errors for hypothesis testing and confidence intervals after covariate adjustment [105] [106]. | Reporting the precision of a treatment effect estimated using CUPED or the pre-/in-experiment method. |
The strategic integration of covariates is a powerful lever for reducing residual unexplained variability, sharpening the contrast between population means and enriching our understanding of individual variation. While foundational methods like ANCOVA and CUPED offer simplicity and robustness, newer techniques like Overlap Weighting and Doubly Robust estimation provide enhanced efficiency and protection against model misspecification. The most promising developments lie in the intelligent combination of pre-experiment and in-experiment data, offering substantial gains in sensitivity. The choice of strategy must be guided by the research question, data structure, and a careful adherence to methodological principles to avoid bias, ensuring that the pursuit of precision does not come at the cost of accuracy.
Frameworks for Validation: Assessing Bioequivalence and Treatment Personalization
For researchers and drug development professionals, the selection of a bioequivalence (BE) approach is a critical strategic decision in the drug development and regulatory submission process. This guide provides a comparative analysis of the concepts, statistical criteria, and regulatory applications of Average (ABE), Population (PBE), and Individual (IBE) Bioequivalence, contextualized within the framework of population mean versus individual variation research.
Core Concepts and Regulatory Significance
Bioequivalence assessment is a cornerstone of generic drug approval and formulation development, ensuring that a new drug product (test) performs similarly to an approved product (reference) without the need for extensive clinical trials [109]. The evolution from Average Bioequivalence (ABE) to Population Bioequivalence (PBE) and Individual Bioequivalence (IBE) represents a paradigm shift from comparing simple averages to incorporating variance components, addressing the interplay between population-level and individual-level responses [110].
- ABE focuses solely on the comparison of population averages, asking "Are the mean values of the pharmacokinetic (PK) endpoints for the reference and test formulations similar enough?" [111]. It is the most established and widely required method by global regulators [111] [109].
- PBE broadens the scope, asking "Are the full distributions of the PK endpoints similar enough?" [111]. It is particularly important for determining prescribability—the decision to assign a patient one formulation as part of an initial treatment [111] [110].
- IBE represents the most stringent approach, asking if the formulations are sufficiently similar within individuals. This is crucial for assessing switchability—the safety of substituting one formulation for another in a patient already stabilized on a treatment regimen [111] [110].
The "Fundamental Bioequivalence Assumption" underpins all three methods: if two drug products are shown to be bioequivalent in their rate and extent of absorption, they are assumed to be therapeutically equivalent [112]. The choice of BE method directly impacts the level of confidence in this assumption for diverse patient populations and individual patient scenarios.
Comparative Analysis of BE Approaches
The following table summarizes the key characteristics, statistical criteria, and primary applications of ABE, PBE, and IBE.
Table 1: Comprehensive Comparison of Bioequivalence Approaches
| Feature | Average Bioequivalence (ABE) | Population Bioequivalence (PBE) | Individual Bioequivalence (IBE) |
|---|---|---|---|
| Core Question | Are the population means equivalent? [111] | Are the total distributions equivalent? [111] | Are the formulations equivalent within individuals? [110] |
| Primary Concern | Average patient response [110] | Prescribability for drug-naïve patients [111] [110] | Switchability for patients switching formulations [111] [110] |
| Key PK Parameters | AUC (extent of absorption) & Cmax (rate of absorption) [113] [112] | AUC & Cmax [114] | AUC & Cmax [114] |
| Statistical Metric | 90% Confidence Interval of the ratio of geometric means (T/R) must be within 80-125% [113] [112]. | Composite metric of mean difference and total variance [110]. | Composite metric of mean difference, subject-by-formulation interaction, and within-subject variances [110]. |
| Variance Consideration | Does not directly compare variances [109]. | Compares total variance (within- + between-subject) of T and R [111] [110]. | Compares within-subject variances of T and R and assesses subject-by-formulation interaction (σD) [110]. |
| Regulatory Status | Standard for most drugs; globally accepted [111] [109]. | Considered for new drug substances and certain special cases; not standard for generics [114]. | Historically debated; not commonly required for standard generic approval [114]. |
| Typical Study Design | 2-treatment, 2-period crossover (2x2) [110] [114]. | 2-treatment, 2-period crossover or replicated designs [114]. | Replicated crossover designs (e.g., 3 or 4 periods) [111] [110]. |
Focus on Highly Variable Drugs and Reference-Scaling
For Highly Variable Drugs (HVDs), defined by an within-subject coefficient of variation (CV) greater than 30%, the standard ABE approach often requires impractically large sample sizes to demonstrate equivalence [113] [115]. To address this, a scaled approach called Reference-scaled Average Bioequivalence (RSABE) is employed [113].
RSABE widens the bioequivalence acceptance limits in proportion to the within-subject variability (SWR) of the reference product. This scaling acknowledges that for highly variable drugs, wider differences in PK parameters may not be clinically significant [113]. Regulatory bodies have specific requirements for its application, as shown in the table below.
Table 2: Regulatory Criteria for Reference-Scaled Average Bioequivalence (RSABE)
| Parameter | Agency | Condition (Within-subject SD, sWR) | Acceptance Criteria |
|---|---|---|---|
| AUC | U.S. FDA | < 0.294 | Standard ABE (90% CI within 80-125%) |
| ≥ 0.294 | RSABE permitted; CI can be widened; point estimate within 80-125% [113] | ||
| EMA | Any value | Standard ABE (90% CI within 80-125%) only [113] | |
| Cmax | U.S. FDA | < 0.294 | Standard ABE (90% CI within 80-125%) |
| ≥ 0.294 | RSABE permitted; CI can be widened; point estimate within 80-125% [113] | ||
| EMA | < 0.294 | Standard ABE (90% CI within 80-125%) | |
| ≥ 0.294 | RSABE permitted; CI widened up to 69.84-143.19%; point estimate within 80-125% [113] |
Experimental Protocols and Methodologies
The choice of BE approach directly dictates the required clinical study design and statistical analysis plan.
Standard ABE Study Protocol
The standard design for ABE is a two-treatment, two-period, two-sequence crossover study [112] [110].
- Subjects: Healthy volunteers are typically used, assuming BE in them predicts BE in patients [112].
- Randomization: Subjects are randomly allocated to one of two sequences: TR (Test then Reference) or RT (Reference then Test) [110].
- Procedure: Each subject receives both the test and reference formulations in separate periods, with adequate washout between doses to prevent carryover effects [112].
- Bioanalysis: Blood samples are collected at predetermined times post-dose to construct a concentration-time profile [115].
- Endpoint Calculation: Key PK parameters, AUC and Cmax, are calculated for each subject and formulation using non-compartmental analysis [113].
- Statistical Analysis: The AUC and Cmax values are log-transformed and analyzed using a linear mixed-effects model. ABE is concluded if the 90% confidence interval for the ratio of geometric means (T/R) for both parameters falls entirely within the 80-125% range [112].
Replicated Crossover Design for IBE/PBE
Both IBE and PBE require replicated crossover designs where subjects receive the same formulation at least twice, which is necessary to estimate within-subject variances for both formulations and the subject-by-formulation interaction [111] [110].
Common designs include:
- 3-period designs: Such as TRR, RTR, or RRT (partially replicated) [113] [111].
- 4-period designs: Such as TRTR or RTRT (fully replicated) [113] [111].
The statistical analysis employs more complex linear mixed models. For example, the FDA-preferred model for a replicated design does not assume homogeneity of variances [111]:
log(endpoint) ~ formulation + sequence + period + (formulation + 0 | id)
The IBE and PBE metrics are composite (see Table 1), and bioequivalence is claimed if the 95% upper confidence bound for the metric is less than a pre-defined regulatory constant (θI or θP), and the point estimate of the geometric mean ratio is within 80-125% [110].
Visualizing Bioequivalence Decision Pathways
The following diagram illustrates the logical workflow for selecting and applying different bioequivalence approaches, highlighting the key decision points and criteria.
Essential Research Tools and Reagents
Successfully conducting BE studies requires a combination of specialized statistical software, analytical tools, and carefully controlled materials.
Table 3: Research Reagent Solutions for Bioequivalence Studies
| Tool / Reagent | Function / Description | Application in BE Studies |
|---|---|---|
| Phoenix WinNonlin | Industry-standard software for PK/PD data analysis [113]. | Used for non-compartmental analysis to calculate primary PK endpoints (AUC, Cmax); supports RSABE analysis via templates [113]. |
| Bioequivalence Package (Pumas) | A specialized package in the Pumas software platform for BE analysis [111]. | Performs statistical analysis for ABE, PBE, and IBE; supports a wide array of standard and replicated study designs [111]. |
| SAS Proc Mixed | A powerful procedure in SAS for fitting linear mixed models [110]. | The historical gold-standard for analyzing complex variance structures in IBE and PBE studies [110]. |
| Validated Bioanalytical Method | An analytical method (e.g., LC-MS/MS) validated to FDA/EMA guidelines. | Quantifies drug concentrations in biological fluids (e.g., plasma) with required specificity, accuracy, and precision to generate reliable PK data. |
| Pharmaceutical Equivalents | Test and Reference products with identical active ingredient(s), dosage form, strength, and route of administration [112] [109]. | The fundamental materials under comparison; must be pharmaceutically equivalent for a standard BE study [112]. |
In pharmaceutical formulation development, demonstrating bioequivalence (BE) is a critical step for the approval of generic drugs or new formulations of existing drugs. BE assessment ensures that the test product (e.g., a generic) is equivalent to the reference product (e.g., the innovator) in its rate and extent of absorption, thereby establishing therapeutic equivalence [112] [109]. The core dilemma in BE analysis lies in choosing a statistical approach that balances the simplicity of comparing population means against the complexity of accounting for individual variation in drug response. This choice is not merely statistical but has profound implications for drug safety, efficacy, and regulatory strategy [110].
The Fundamental Bioequivalence Assumption underpins all BE assessments: if two drug products are shown to be bioequivalent, it is assumed that they will reach the same therapeutic effect [112]. However, the verification of this assumption is complex. For instance, drug absorption profiles might be similar without guaranteeing therapeutic equivalence, or they might differ while still yielding equivalent therapeutic outcomes [112]. This complexity has given rise to three primary statistical approaches for BE assessment: Average Bioequivalence (ABE), Population Bioequivalence (PBE), and Individual Bioequivalence (IBE). This guide provides an objective comparison of these methodologies, detailing their performance, underlying experimental protocols, and appropriate applications within formulation development.
Understanding the BE Approaches: Definitions, Metrics, and Regulatory Context
Average Bioequivalence (ABE)
ABE is the longstanding, most widely used standard for establishing BE. It focuses exclusively on comparing the population average values of key pharmacokinetic (PK) parameters, such as the area under the concentration-time curve (AUC) and the maximum concentration (Cmax), between the test (T) and reference (R) products [112] [110] [109].
- Key Metric: ABE utilizes the "80/125 rule." After log-transformation of the PK data, the 90% confidence interval for the ratio of the geometric means (T/R) for AUC and Cmax must fall entirely within the bioequivalence limits of 80% to 125% [112].
- Regulatory Preference: ABE is the standard method recommended by the European Medicines Agency (EMA) and is accepted globally for most drug products [116] [109].
- Limitation: A significant concern with ABE is that it ignores the variance of the PK parameters. It is possible for a test product to have a mean bioavailability within the 80-125% range while exhibiting higher variability than the reference product. This could potentially lead to a higher-than-acceptable number of individuals experiencing very high or very low drug exposure, raising safety or efficacy concerns [110] [109].
Population Bioequivalence (PBE)
PBE extends the comparison beyond just averages to include the total variability (both within- and between-subject) of the test and reference products. It is primarily concerned with prescribability – assuring a physician that a drug-naïve patient can be prescribed either the test or reference product with an equal expectation of safety and efficacy [110].
- Key Metric: The PBE metric is a composite measure that incorporates the difference between the means and the difference between the total variances of the two products [110]. The following equation is used: θP = (μT - μR)² + (σ²TT - σ²TR) / max(σ²TR, σ²₀) where μT and μR are the population means, σ²TT and σ²TR are the total variances of the test and reference products, and σ²₀ is a constant scaling factor [110]. A one-sided 95% confidence interval for this metric must be below a predefined regulatory limit.
- Regulatory Preference: The U.S. Food and Drug Administration (FDA) places a stronger emphasis on PBE, particularly for certain complex drug products [116] [109].
- Implication: PBE is more restrictive than ABE if the reference product has low variability. Conversely, it can be less restrictive than ABE if the reference product is highly variable, provided the test product's variability is not greater [116].
Individual Bioequivalence (IBE)
IBE is the most stringent approach, as it assesses both the mean difference and the within-subject variability, and specifically accounts for the subject-by-formulation interaction. This is a measure of whether a subject's response to the test product is predictably different from their response to the reference product. IBE addresses switchability – assuring that a patient stabilized on one formulation (e.g., the reference) can be safely switched to another (e.g., the generic) without a change in therapeutic outcome [110].
- Key Metric: The IBE metric includes components for the mean difference, subject-by-formulation interaction (σD²), and the difference in within-subject variances (σ²WT - σ²WR) [110]. The equation is: θI = (μT - μR)² + σD² + (σ²WT - σ²WR) / max(σ²WR, σ²W₀) Similar to PBE, a one-sided confidence interval is calculated and compared to a regulatory bound.
- Application: IBE is critical when considering drugs with a narrow therapeutic index or when switching between formulations in a clinical setting is common.
Table 1: Core Characteristics of ABE, PBE, and IBE
| Feature | Average Bioequivalence (ABE) | Population Bioequivalence (PBE) | Individual Bioequivalence (IBE) |
|---|---|---|---|
| Primary Question | Are the population averages equivalent? | Can a new patient be prescribed either product? | Can a patient be switched from one product to the other? |
| Core Concern | Prescribability | Prescribability | Switchability |
| Key Metric Components | Difference in means | Difference in means + Difference in total variances | Difference in means + Subject-by-formulation interaction + Difference in within-subject variances |
| Regulatory Scaling | No (Constant Limits) | Yes (Reference-scaled) | Yes (Reference-scaled) |
| Handles HVDP | Poorly, requires large sample size | Better, can use reference-scaling | Better, can use reference-scaling |
Methodologies and Experimental Protocols
The choice of BE approach directly dictates the design of the clinical study, the data collection process, and the statistical analysis plan.
Study Design
- ABE Studies: Typically employ a standard two-sequence, two-period (2x2) crossover design [112]. In this design, subjects are randomly assigned to one of two sequences. One sequence receives the test product in period 1 and the reference in period 2, while the other sequence receives the treatments in reverse order. A washout period separates the two periods to eliminate carryover effects.
- PBE and IBE Studies: Require more complex replicate designs [110]. Common designs include:
- 4-period replicate: TRTR or RTRT sequences, where each subject receives each formulation twice.
- 3-period replicate: TRT or RTR sequences. These designs are necessary because estimating within-subject variances and the subject-by-formulation interaction requires each subject to be exposed to the same formulation on more than one occasion [110].
Sample Size and Subject Selection
- ABE: Sample sizes are calculated based on the expected within-subject variability and the desired power to show that the confidence interval lies within the 80-125% limits. For drugs with low variability, 20-40 subjects may suffice.
- PBE/IBE: Generally require larger sample sizes than ABE due to the need to estimate variance components with precision. The FDA recommends a minimum of 12 subjects for IBE and 18 for PBE in pilot studies, but final studies often require more [110]. Studies for Highly Variable Drugs and Products (HVDP) require even larger sample sizes for ABE, a problem that can be mitigated by the scaled approaches of PBE and IBE [116].
Statistical Analysis Workflow
The statistical analysis for all methods typically involves a linear mixed-effects model. The analysis proceeds through several key stages, with the choice of model and endpoints differing between ABE and the variance-component approaches (PBE/IBE).
Diagram 1: Statistical analysis workflows for ABE versus PBE/IBE.
Decision Framework: When to Use Which Approach
Selecting the appropriate BE approach is a strategic decision based on the drug's properties, the development goals, and regulatory requirements.
Table 2: Decision Matrix for Selecting a Bioequivalence Approach
| Scenario / Product Characteristic | Recommended Approach | Rationale and Supporting Evidence |
|---|---|---|
| New Generic for Drug with Wide Therapeutic Index | ABE | The standard and most cost-effective method. Sufficient for ensuring comparable average exposure for most small molecule drugs [109]. |
| Drugs with High Variability (HVDP) | PBE (or IBE) | ABE power drops off significantly when within-product CV% exceeds ~15-30%, often requiring prohibitively large sample sizes. PBE's reference-scaling is better suited for such products [116] [117]. |
| Orally Inhaled and Nasal Drug Products | PBE | The FDA often recommends PBE for locally acting drugs delivered via inhalation or nasal sprays, as it ensures equivalence not only in averages but also in the population distribution of key in vitro performance measures [116] [117]. |
| Narrow Therapeutic Index Drugs | Consider IBE | While not always mandated, IBE provides the highest assurance of switchability, minimizing the risk of adverse events or loss of efficacy when a patient switches products. |
| Formulations Where Patient Switching is Anticipated | IBE | If the generic is expected to be used as a substitute for the brand in a pharmacy, IBE's assessment of subject-by-formulation interaction directly addresses switchability [110]. |
| Products with Non-Negligible Between-Batch Variability | Emerging Methods (e.g., BBE) | Recent research on Between-Batch Bioequivalence (BBE) suggests that neglecting batch variability can inflate Type I error. BBE may be more efficient in these cases, though not yet standard [116] [117]. |
The Scientist's Toolkit: Essential Reagents and Materials for BE Studies
Table 3: Key Research Reagent Solutions for Bioequivalence Studies
| Item / Solution | Function in BE Studies |
|---|---|
| Validated Bioanalytical Method (e.g., LC-MS/MS) | To accurately and precisely quantify the concentration of the active drug and/or its metabolites in biological fluids (e.g., plasma, serum) over time. This is the foundation of all PK parameter estimation. |
| Clinical Protocol with Pre-Specified Statistical Analysis Plan (SAP) | To define the study objectives, design (crossover/replicate), sample size, inclusion/exclusion criteria, and detailed statistical methods before data collection, ensuring regulatory integrity. |
| Stable Isotope-Labeled Internal Standards | Used in mass spectrometry-based bioanalysis to correct for matrix effects and variability in sample preparation, thereby improving the accuracy and precision of concentration measurements. |
| Pharmacokinetic Data Analysis Software (e.g., WinNonlin, NONMEM) | To perform non-compartmental analysis for deriving primary PK endpoints (AUC, Cmax) and to conduct complex statistical modeling for ABE, PBE, and IBE. |
| Software for Linear Mixed-Effects Modeling (e.g., SAS Proc Mixed, R) | Essential for the complex variance-component estimation required for PBE and IBE analysis, as these methods go beyond simple mean comparisons [110]. |
The choice between ABE, PBE, and IBE is a fundamental strategic decision in formulation development. ABE, with its focus on population means, remains the workhorse for the majority of generic small-molecule drugs due to its simplicity and regulatory acceptance. However, its inability to account for variance and individual response is a significant limitation. PBE and IBE offer more robust frameworks by incorporating variance components, with PBE safeguarding prescribability for new patients and IBE ensuring switchability for existing patients.
The trend in regulatory science is moving towards approaches that more fully account for the true variability in drug products and patient responses. While practical considerations of cost and complexity currently limit the widespread use of PBE and IBE, they represent a more scientifically complete paradigm for demonstrating therapeutic equivalence. Formulation scientists must therefore be well-versed in all three approaches, applying them judiciously based on the specific risk-benefit profile of the drug product under development to ensure both regulatory success and patient safety.
Statistical and Regulatory Hurdles in Proving Switchability and Prescribability
In drug development, a fundamental tension exists between demonstrating average treatment effects for populations and addressing individual variation in treatment response. Switchability and prescribability represent two critical concepts in bioequivalence and drug development that sit at the heart of this statistical challenge. Switchability refers to the ability of a patient to switch between drug products without experiencing significant changes in safety or efficacy, while prescribability addresses whether a new drug product can be reliably prescribed to new patients in place of an existing treatment.
The core statistical hurdle lies in the fact that traditional hypothesis testing primarily focuses on detecting differences in population means, while individual variation requires understanding of population distributions and their overlap. This article examines both the statistical methodologies for comparing population means and the regulatory frameworks that are evolving to address these challenges in modern drug development.
Statistical Foundations: Comparing Population Means
The Aspin-Welch t-Test for Independent Populations
The comparison of two independent population means is one of the most common statistical procedures in pharmaceutical research. The test comparing two independent population means with unknown and possibly unequal population standard deviations is called the Aspin-Welch t-test [118] [119].
When we develop hypothesis tests for means, we begin with the Central Limit Theorem, which tells us that the distribution of sample means approaches normal distribution regardless of the underlying population distribution. For two samples, we create a new random variable—the difference between the sample means—which also follows a normal distribution according to the Central Limit Theorem [118].
The test statistic (t-score) is calculated as follows [118] [119]:
[tc= \frac{(\overline{x}1-\overline{x}2)-\delta0}{\displaystyle\sqrt{\frac{(s1)^2}{n1}+\frac{(s2)^2}{n2}}}]
Where:
- (\overline{x}1) and (\overline{x}2) are the sample means
- (s1) and (s2) are the sample standard deviations
- (n1) and (n2) are the sample sizes
- (\delta_0) is the hypothesized difference between population means (typically 0)
The standard error of the difference in sample means is [120] [119]:
[\sqrt{\frac{(s1)^2}{n1}+\frac{(s2)^2}{n2}}]
The degrees of freedom for this test use a complicated formula, though computers and calculators can compute it easily [119]. The conditions required for using this two-sample t-interval or test include: the two random samples must be independent and representative, and the variable should be normally distributed in both populations (though this requirement can be relaxed with larger sample sizes due to the Central Limit Theorem) [120].
Table 1: Key Statistical Tests for Comparing Population Means
| Test Type | Formula | When to Use | Assumptions |
|---|---|---|---|
| Aspin-Welch t-Test | (t= \frac{(\overline{x}1-\overline{x}2)-\delta0}{\sqrt{\frac{(s1)^2}{n1}+\frac{(s2)^2}{n_2}}}) | Comparing means of two independent groups with unknown, potentially unequal variances | Independent samples, normality (or large n), similar distributions |
| Confidence Interval for Difference | ((\overline{x1}-\overline{x2})± Tc\cdot \sqrt{\frac{s1^2}{n1}+\frac{s2^2}{n_2}}) | Estimating the size of population mean difference when results are statistically significant | Same as t-test assumptions |
| Two-Proportion Z-Test | (Z=\frac{(\hat{p}1-\hat{p}2)-0}{\sqrt{\hat{p}(1-\hat{p})(\frac{1}{n1}+\frac{1}{n2})}) | Comparing proportions between two independent groups | Independent samples, sufficient sample size (np≥10, n(1-p)≥10) |
Confidence Intervals for Mean Differences
When sample evidence leads to rejecting the null hypothesis, researchers often calculate a confidence interval to estimate the size of the population mean difference [120]. The confidence interval takes the form:
[(\overline{x1}-\overline{x2})± Tc\cdot \sqrt{\frac{s1^2}{n1}+\frac{s2^2}{n_2}}]
Where (T_c) is the critical T-value from the t-distribution based on the desired confidence level and degrees of freedom.
Table 2: Example of Two-Sample T-Interval Calculation
| Parameter | Sample 1 (Group A) | Sample 2 (Group B) | Calculation |
|---|---|---|---|
| Sample Size | n₁ = 45 | n₂ = 27 | - |
| Sample Mean | (\overline{x_1}) = 850 | (\overline{x_2}) = 719 | (\overline{x1}-\overline{x2}) = 131 |
| Sample Standard Deviation | s₁ = 252 | s₂ = 322 | - |
| Standard Error | - | - | (\sqrt{\frac{252^2}{45}+\frac{322^2}{27}} \approx 72.47) |
| Critical T-value (95%) | - | - | 1.6790 (df = 45) |
| Margin of Error | - | - | 1.6790 × 72.47 ≈ 122 |
| 95% Confidence Interval | - | - | 131 ± 122 = (9, 253) |
Visualizing the Statistical Testing Workflow
The following diagram illustrates the logical workflow for conducting hypothesis tests comparing two population means:
Hypothesis Testing Workflow for Two Means
Regulatory Frameworks and Evidence Requirements
The Evolving Regulatory Landscape for 2025
The regulatory environment for drug development is undergoing significant transformation, with several key changes taking effect in 2025 [121]:
- Enhanced Data Integrity and Traceability: New ICH E6(R3) guidelines emphasize greater scrutiny on data management, including detailed documentation throughout a sample's lifecycle.
- Single IRB Review for Multicenter Studies: The FDA is harmonizing guidance on single IRB reviews for multicenter studies to streamline ethical review.
- Increased Use of AI and Real-World Data: The FDA will publish draft regulatory guidance on using AI for regulatory decision-making.
- Focus on Diverse Participant Enrollment: Regulatory agencies are increasing focus on regulations for vulnerable populations to improve participant diversity.
Novel Approaches for Rare Diseases and Complex Scenarios
For rare diseases with very small patient populations (generally fewer than 1,000 patients in the United States), the FDA has introduced the Rare Disease Evidence Principles (RDEP) to provide greater speed and predictability in therapy review [122]. This process acknowledges the difficulty of conducting multiple traditional clinical trials for rare diseases and allows for approval based on one adequate and well-controlled study plus robust confirmatory evidence, which may include:
- Strong mechanistic or biomarker evidence
- Evidence from relevant non-clinical models
- Clinical pharmacodynamic data
- Case reports, expanded access data, or natural history studies
The BenchExCal Framework for Regulatory Confidence
The Benchmark, Expand, and Calibration (BenchExCal) approach provides a structured method for increasing confidence in database studies used to support regulatory decisions [123]. This methodology addresses the challenge of emulating randomized controlled trials (RCTs) with real-world data by:
- Benchmarking: Demonstrating the ability to closely emulate trial(s) used for an initial indication
- Expanding: Using learnings from the initial emulation to plan database studies for expanded populations, subgroups, or outcomes
- Calibration: Applying sensitivity analysis to integrate knowledge of divergence observed in the initial RCT-database study pair
This approach is particularly valuable for supporting supplemental indications beyond existing effectiveness claims, where it can increase confidence in the validity of findings from cohort studies conducted using healthcare databases [123].
Table 3: Regulatory Evidence Frameworks for Drug Development
| Framework | Key Features | Application Context | Evidence Requirements |
|---|---|---|---|
| Traditional RCT | Randomized controlled design, strict inclusion/exclusion criteria | Pre-market approval for new drugs | Two adequate and well-controlled studies |
| Rare Disease Evidence Principles (RDEP) | Flexible evidence standards, genetic defect focus | Rare diseases with small populations (<1000 US patients) | One adequate study plus confirmatory evidence |
| BenchExCal Approach | Database study benchmarking against existing RCTs | Expanded indications for marketed drugs | Database study emulation with calibration |
| Real-World Evidence (RWE) | Healthcare database studies, pragmatic designs | Post-market safety and effectiveness | Causal inference methods, bias control |
Experimental Protocols and Methodologies
Standard Protocol for Two-Sample Mean Comparison
The following detailed methodology outlines the standard approach for comparing two independent population means, as referenced in statistical literature [118] [119]:
Objective: To determine if there is a statistically significant difference between the means of two independent populations.
Materials and Sample Collection:
- Select two independent simple random samples from two distinct populations
- Ensure samples are representative of their respective populations
- Record sample sizes (n₁ and n₂), sample means ((\overline{x}1) and (\overline{x}2)), and sample standard deviations (s₁ and s₂)
Procedure:
- State the null hypothesis (H₀: μ₁ = μ₂) and alternative hypothesis (Hₐ: μ₁ ≠ μ₂, μ₁ > μ₂, or μ₁ < μ₂)
- Verify conditions for inference:
- Independence: Both samples are collected independently
- Normality: The variable is normally distributed in both populations, OR both sample sizes are sufficiently large (n ≥ 30 for each group)
- For smaller samples, check histograms or dotplots for extreme skew or outliers
- Calculate the standard error: (\sqrt{\frac{(s1)^2}{n1}+\frac{(s2)^2}{n2}})
- Compute the test statistic: (t= \frac{(\overline{x}1-\overline{x}2)-0}{\sqrt{\frac{(s1)^2}{n1}+\frac{(s2)^2}{n2}}})
- Determine the degrees of freedom using the Aspin-Welch formula
- Calculate the p-value using the t-distribution with the appropriate degrees of freedom
- Make a decision based on comparison of p-value to significance level (α)
- If rejecting the null hypothesis, compute a confidence interval to estimate the effect size
Interpretation:
- Report the conclusion in the context of the original research question
- Discuss both statistical and practical significance of findings
- Acknowledge limitations, including potential for Type I or Type II errors
Visualizing the Regulatory Benchmarking Process
The following diagram illustrates the BenchExCal methodology for regulatory benchmarking:
BenchExCal Regulatory Benchmarking Process
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Tools for Statistical Comparison Studies
| Tool/Reagent | Function/Purpose | Application Context |
|---|---|---|
| Statistical Software (R, Python, SAS) | Implementation of Aspin-Welch t-test and confidence interval calculations | All statistical comparison studies |
| Electronic Health Record (EHR) Systems | Source of real-world data for database studies | Observational studies, benchmark exercises |
| Data Standardization Protocols | Ensure consistent measurement across study sites | Multicenter trials, real-world evidence generation |
| Sample Size Calculation Tools | Determine minimum sample needed for adequate power | Study design phase |
| Bias Assessment Frameworks | Evaluate potential confounding in observational studies | Database study design and interpretation |
| Biomarker Assay Kits | Quantitative measurement of physiological endpoints | Clinical trials, mechanistic studies |
| Data Integrity Solutions | Maintain chain of custody and audit trails | Regulatory submissions requiring ICH E6(R3) compliance |
| AI/ML Platforms for Data Analysis | Pattern recognition in complex datasets | Large database analysis, predictive modeling |
The challenges of proving switchability and prescribability highlight the ongoing tension between population-level statistics and individual variation in drug development. The statistical methods for comparing population means, particularly the Aspin-Welch t-test for independent samples, provide a foundation for demonstrating average treatment effects. However, these methods must be applied with careful attention to their assumptions and limitations.
Meanwhile, regulatory science is evolving to address these challenges through frameworks like the Rare Disease Evidence Principles and BenchExCal methodology, which allow for more flexible evidence generation while maintaining scientific rigor. As we move toward 2025, with increased use of AI, real-world evidence, and more complex trial designs, the statistical and regulatory hurdles in proving switchability and prescribability will continue to require sophisticated approaches that balance population means with individual variation.
Successful navigation of this landscape demands both technical expertise in statistical methodology and strategic understanding of evolving regulatory pathways. Researchers and drug development professionals must stay abreast of these changes to efficiently bring new treatments to patients while maintaining the highest standards of evidence and safety.
The foundational premise of traditional evidence-based medicine, which relies on population means derived from large randomized controlled trials (RCTs), is increasingly being challenged by the recognition of significant individual variation in treatment response. The core thesis of this review posits that while population-level evidence provides a crucial starting point for clinical decision-making, it often fails to account for the vast heterogeneity in treatment effects observed across individuals, thereby compelling the adoption of more personalized approaches [124]. This paradigm shift is driven by growing recognition that the "average" patient represented in clinical trials is a statistical abstraction that may not correspond to any single individual in real-world practice [125]. The limitations of this one-size-fits-all approach are particularly evident in complex conditions like cancer, mental health disorders, and critical illness, where molecular heterogeneity and individual differences in treatment response are the rule rather than the exception [126] [124].
The practice of personalized medicine represents a fundamental transformation in healthcare delivery, moving away from population-wide generalizations toward treatments tailored to an individual's unique genetic makeup, environmental influences, and lifestyle factors [127] [128]. This approach leverages advancements in genomic technologies, biomarker discovery, and data analytics to develop more precise therapeutic interventions that account for individual variation [126]. The clinical application of personalized approaches has demonstrated superior response rates and reduced adverse effects compared to traditional methods across various medical specialties, particularly in oncology, psychiatry, and cardiovascular medicine [127]. However, the implementation of personalized strategies faces significant challenges, including methodological limitations in clinical trials, difficulties in validating biomarkers, and practical barriers to integration into routine clinical workflows [126] [124].
Methodological Frameworks: Comparing Research Approaches
Traditional Nomothetic Approaches
Traditional clinical research predominantly employs nomothetic approaches that focus on identifying universal principles applicable to populations. These methodologies rely heavily on group-level statistics and aggregate data to draw inferences about treatment efficacy, with the RCT considered the gold standard for generating evidence [125]. In this framework, individual variability is often treated as statistical noise that must be controlled or minimized to detect population-level effects. The primary analytical methods involve comparing population means between treatment and control groups, with statistical significance (typically p < 0.05) serving as the benchmark for establishing treatment efficacy [129]. This approach provides valuable information about what works on average but offers limited guidance for predicting individual treatment responses [125] [124].
The dominance of nomothetic approaches has led to a clinical evidence base characterized by rigid treatment protocols and standardized guidelines derived from population averages. While this paradigm has produced important therapeutic advances, it increasingly faces methodological and philosophical challenges. As noted in critical care literature, "the idea that the evidence is at our fingertips and readily available to support bedside decision making is an illusion" [124]. This recognition stems from the fundamental limitation that population-level evidence does not automatically translate to individual patients, particularly when significant heterogeneity of treatment effects exists within the studied population [124]. Furthermore, traditional trials often oversimplify clinical complexity through stringent inclusion and exclusion criteria that create homogenized patient populations unrepresentative of real-world clinical practice [124].
Emerging Idiographic and Precision Approaches
In contrast to nomothetic methods, idiographic approaches focus on intensive study of individuals through methodologies such as single-subject designs and N-of-1 trials [125]. These approaches prioritize understanding within-individual processes and patterns of change over time, treating each patient as their own control [125]. While offering rich insights into individual trajectories, traditional idiographic approaches have faced limitations in generalizability and throughput. The emerging field of precision medicine seeks to bridge this methodological divide by combining large-scale molecular profiling with advanced analytics to develop personalized prediction models that can inform treatment selection for individuals [130] [126].
Modern precision approaches leverage technological advances in genomic sequencing, proteomics, and bioinformatics to identify molecular subtypes within seemingly homogeneous diagnostic categories [126]. These methodologies enable a more nuanced understanding of disease mechanisms and treatment responses that accounts for biological heterogeneity. Furthermore, the integration of artificial intelligence and machine learning allows for analysis of complex multidimensional data to identify patterns and predictors of treatment response at the individual level [130] [131]. Rather than replacing population-level evidence, these approaches seek to augment it by enabling clinicians to match the right treatment to the right patient based on a more comprehensive understanding of individual differences [126].
Table 1: Comparison of Research Approaches in Personalization
| Feature | Traditional Nomothetic Approach | Emerging Precision Approach |
|---|---|---|
| Primary Focus | Population means and group-level effects | Individual variation and heterogeneous treatment effects |
| Core Methodology | Randomized controlled trials, meta-analyses | Genomic profiling, biomarker discovery, predictive algorithms |
| Statistical Framework | Null hypothesis significance testing, comparison of means | Machine learning, multilevel modeling, mixture models |
| Patient Selection | Broad inclusion criteria to enhance generalizability | Stratification by molecular subtypes or predictive biomarkers |
| Treatment Assignment | Standardized protocols based on population evidence | Algorithm-guided selection based on individual characteristics |
| Outcome Measurement | Group averages on primary endpoints | Individual response patterns, prediction of personal outcomes |
| Key Limitations | May obscure heterogeneous treatment effects | Require large sample sizes, complex validation, higher costs |
Clinical Evidence: Quantitative Comparisons of Personalization Versus Standard Care
Oncology Applications
The most compelling evidence for personalized medicine comes from oncology, where molecular profiling and targeted therapies have fundamentally transformed treatment paradigms across multiple cancer types. A systematic review of personalized approaches across various diseases, including cancer, demonstrated significantly greater response rates ranging from 48.7% to 87% compared to traditional methods, alongside substantially lower adverse drug reactions [127]. These improvements stem from the ability to match specific therapeutic agents to the molecular drivers of an individual's cancer rather than applying histology-based standard treatments indiscriminately.
The clinical impact of genomic profiling in oncology is substantiated by multiple studies. Tsimberidou et al. (2017) conducted a retrospective study of 1,436 patients with advanced cancer who underwent comprehensive genomic profiling [126]. Their findings revealed that among the 637 patients with actionable genetic aberrations, those who received molecularly targeted therapy (n=390) demonstrated significantly improved outcomes compared to those receiving unmatched treatments, including superior response rates (11% vs. 5%), longer failure-free survival (3.4 vs. 2.9 months), and improved overall survival (8.4 vs. 7.3 months) [126]. Similarly, in non-small cell lung cancer (NSCLC), Hughes et al. (2022) demonstrated that targeted therapy based on molecular profiling significantly improved overall survival compared to standard approaches (28.7 vs. 6.6 months) [126]. These findings highlight the profound impact of personalization in matching treatments to individual tumor characteristics.
Mental Health Applications
In mental health care, personalization has emerged as a promising approach to address the substantial heterogeneity in treatment response that has long plagued the field. The precision mental health framework utilizes routine outcome monitoring, predictive algorithms, and systematic feedback to inform treatment selection and adaptation for individual patients [130]. This data-driven approach acknowledges that while numerous evidence-based interventions exist for conditions like depression, their effectiveness varies considerably across individuals, creating a compelling rationale for personalization strategies that can optimize treatment matching [130].
Research by Delgadillo and Lutz (2020) has demonstrated that precision mental health tools can be effectively integrated throughout the care process, spanning prevention, diagnosis, patient-clinician matching, treatment selection, and ongoing adaptation [130]. These approaches leverage large datasets of previously treated patients to develop algorithms that provide personalized clinical recommendations, enabling clinicians to identify optimal interventions based on individual patient profiles rather than population averages. The implementation of such personalized approaches has shown potential to enhance treatment outcomes, particularly for patients who do not respond to standard first-line interventions [130].
Cross-Domain Evidence
Beyond oncology and mental health, personalized approaches have demonstrated efficacy across diverse medical specialties. In cardiovascular medicine, genetic screening enables more accurate assessment of individual susceptibility to heart diseases, facilitating earlier and more targeted preventive interventions [127]. Similarly, applications in autoimmune diseases, neurology, and metabolic conditions have shown promising results, though the evidence base in these domains remains less developed than in oncology [127]. The consistent theme across specialties is that personalized approaches yield superior outcomes when they successfully account for relevant biological or psychological heterogeneity that moderates treatment response.
Table 2: Quantitative Outcomes of Personalized vs. Standard Approaches Across Medical Specialties
| Medical Specialty | Personalized Approach | Response Rate (%) | Standard Approach | Response Rate (%) | Key Findings |
|---|---|---|---|---|---|
| Oncology (Various) | Molecularly targeted therapy based on genomic profiling | 48.7-87.0 [127] | Conventional chemotherapy | Not specified | Significantly improved response rates and reduced adverse effects [127] |
| Oncology (NSCLC) | EGFR inhibitors for EGFR-mutant NSCLC | ~70 [127] | Conventional chemotherapy | Not specified | Substantial improvement in response; overall survival of 24 months [127] |
| Psychiatry | Pharmacogenomic-guided antidepressant therapy | Significantly greater [127] | Traditional trial-and-error approach | Not specified | Improved response rates and reduced adverse drug reactions [127] |
| Critical Care | Phenotype-guided therapy | Emerging approach [124] | Standardized protocols | Not specified | Potential to address heterogeneity of treatment effects in syndromes like ARDS and sepsis [124] |
Key Experimental Methodologies in Personalization Research
Genomic Profiling and Biomarker Validation
The cornerstone of personalized medicine in oncology and other specialties is comprehensive genomic profiling, which enables identification of actionable mutations and predictive biomarkers that guide treatment selection. The standard methodology involves next-generation sequencing (NGS) of tumor tissue or liquid biopsies to characterize the molecular landscape of an individual's disease [126]. The analytical workflow typically begins with sample acquisition, followed by DNA/RNA extraction, library preparation, sequencing, bioinformatic analysis, and clinical interpretation [126]. Validation of identified variants through orthogonal methods (e.g., PCR, Sanger sequencing) is critical before implementing findings in clinical decision-making.
The critical methodological consideration in genomic profiling is the distinction between actionable and non-actionable findings. Actionable mutations are those with validated associations with specific targeted therapies, such as EGFR mutations in NSCLC or BRAF V600E mutations in melanoma [126]. The evidence supporting these associations derives from both prospective clinical trials and real-world evidence databases that aggregate outcomes from patients receiving matched therapies. Recent advances include the integration of multi-omics approaches that combine genomic, transcriptomic, proteomic, and metabolomic data to create more comprehensive molecular profiles [131]. These sophisticated methodologies provide a richer understanding of disease biology but introduce additional complexity in data interpretation and clinical application.
Adaptive Platform Trials
Traditional RCTs face significant limitations for evaluating personalized approaches, particularly their inflexible structure and inability to efficiently test multiple biomarker-guided hypotheses simultaneously. Adaptive platform trials (APTs) have emerged as a innovative methodology designed to address these limitations [130]. These trials employ a master protocol that allows for continuous evaluation of multiple interventions against a common control group, with interventions entering or leaving the platform based on predefined decision algorithms [130]. This flexible structure enables more efficient evaluation of targeted therapies in biomarker-defined subgroups.
The "leapfrog" trial design represents a specialized form of APT that utilizes Bayesian statistics to make sequential comparisons against the most successful treatment identified thus far [130]. This approach offers advantages in reduced sample size requirements and increased efficiency in identifying optimal treatments for specific patient subpopulations. Methodologyically, APTs require sophisticated statistical planning, including pre-specified adaptation rules, Bayesian analytical frameworks, and robust data monitoring systems [130]. While methodologically complex, these trial designs provide a more efficient framework for developing evidence to support personalized treatment approaches compared to traditional parallel-group RCTs.
Single-Subject Experimental Designs
In behavioral medicine and mental health, single-subject designs represent a foundational methodology for personalization research [125]. These designs involve repeated measurement of outcomes within individuals across different conditions (e.g., baseline versus intervention) to establish causal relationships at the individual level [125]. The core methodological principle is that each subject serves as their own control, with visual analysis of time-series data used to evaluate treatment effects. Modern extensions of this approach incorporate experience sampling methods (ESM) that enable intensive longitudinal data collection in naturalistic settings [130].
Recent methodological innovations have focused on combining the strengths of single-subject designs with larger sample sizes to enable both idiographic and nomothetic inferences. This "blended" approach uses large-N datasets and statistical methods such as multilevel modeling to preserve individual-level data while also identifying group-level patterns [125]. Additional analytical techniques include correlational analyses, machine learning, clustering algorithms, and simulation methods that account for individual differences while facilitating broader inferences [125]. These methodological advances address historical limitations of single-subject designs while maintaining their focus on individual variation and patterns of change.
Visualization of Research Approaches and Workflows
Conceptual Framework: Population Mean vs. Individual Variation
The following diagram illustrates the fundamental conceptual relationship between population means and individual variation in treatment response, highlighting how personalized approaches seek to account for heterogeneity that is obscured by aggregate data:
Genomic Profiling Workflow for Personalized Oncology
This diagram outlines the standard experimental workflow for genomic profiling in personalized oncology, from sample collection to clinical decision-making:
The Scientist's Toolkit: Essential Reagents and Technologies
Research Reagent Solutions for Personalization Studies
Table 3: Essential Research Reagents and Technologies for Personalized Medicine Studies
| Category | Specific Products/Technologies | Primary Function | Application in Personalization |
|---|---|---|---|
| Genomic Sequencing | Next-generation sequencing platforms (Illumina), whole genome sequencing kits | Comprehensive molecular profiling | Identification of actionable mutations, biomarker discovery [126] [131] |
| Bioinformatic Tools | Variant calling algorithms, annotation databases (ClinVar, COSMIC) | Analysis and interpretation of genomic data | Distinguishing driver from passenger mutations, clinical decision support [126] |
| Biomarker Testing | Immunohistochemistry assays, PCR-based tests, liquid biopsy kits | Detection of specific molecular alterations | Patient stratification, treatment selection, response monitoring [126] |
| Cell Culture Models | Patient-derived organoids, 3D culture systems | Ex vivo therapeutic testing | Prediction of individual treatment response, functional validation [131] |
| AI/Machine Learning | Predictive algorithms, neural networks, meta-learners | Analysis of complex multimodal data | Treatment outcome prediction, patient stratification, clinical decision support [130] [131] |
Strengths and Limitations of Personalization Evidence
Demonstrated Strengths
The most compelling strength of personalized medicine is its demonstrated ability to improve clinical outcomes across multiple domains. Systematic reviews have consistently shown that personalized approaches yield significantly higher response rates (ranging from 48.7% to 87%) compared to traditional methods [127]. This enhanced efficacy stems from better matching of treatments to individual characteristics, particularly in oncology where targeted therapies directed against specific molecular alterations have produced remarkable improvements in outcomes for biomarker-selected populations [126]. Beyond improved efficacy, personalized approaches have demonstrated reduced adverse effects, as seen in pharmacogenomic-guided prescribing that minimizes adverse drug reactions by accounting for individual metabolic variations [127].
Another significant strength is the ability of personalized approaches to address biological heterogeneity that confounds traditional one-size-fits-all treatments. In conditions like cancer, mental health disorders, and critical illness syndromes, substantial molecular and phenotypic heterogeneity exists beneath surface-level diagnostic categories [126] [124]. Personalized approaches acknowledge this diversity and seek to identify meaningful subgroups that benefit from specific interventions. Furthermore, personalized medicine facilitates a more efficient drug development process by focusing on biomarker-defined populations more likely to respond to investigational therapies, potentially reducing trial costs and failure rates [127] [128].
Acknowledged Limitations and Challenges
Despite its promise, the evidence base for personalized medicine faces significant limitations. Many personalized approaches lack validation in large-scale prospective trials, with evidence often derived from retrospective analyses or subgroup findings [124]. This creates uncertainty about the generalizability and robustness of observed effects. Additionally, methodologies for identifying and validating biomarkers remain challenging, with issues of analytic validity, clinical validity, and clinical utility requiring rigorous assessment before implementation [126]. The high costs associated with genomic profiling and targeted therapies also create substantial economic barriers to widespread implementation [126] [128].
Beyond methodological and economic challenges, personalized medicine faces conceptual limitations in its current implementation. The predominant focus on molecular characteristics often overlooks important environmental, psychological, and social determinants of treatment response [130]. Furthermore, excessive reliance on algorithmic decision-making risks diminishing the importance of clinical expertise and the therapeutic relationship, which remain essential components of effective care [130] [124]. As noted in critical care literature, "Without clinical expertise, practice risks becoming tyrannized by evidence" [124], highlighting the need for balanced integration of personalized approaches with clinical judgment.
The evaluation of clinical evidence for personalization reveals a healthcare paradigm in transition, moving from population-level generalizations toward more individualized approaches that account for biological and psychological heterogeneity. The strengths of personalized medicine—particularly its ability to improve outcomes by matching treatments to individual characteristics—are substantiated by growing evidence across multiple medical specialties [127] [126]. However, significant limitations remain, including methodological challenges in evidence generation, validation of biomarkers, and practical barriers to implementation [126] [124].
The most promising path forward involves the thoughtful integration of both population-based and individualized evidence. Rather than representing opposing paradigms, these approaches complement each other—population data provides the foundational evidence for treatment efficacy, while personalized methods enhance the application of this evidence to individual patients [125] [124]. Future advances will require methodological innovations in trial design, improved biomarker validation frameworks, and greater attention to the practical implementation of personalized approaches in diverse clinical settings [130] [126]. As these developments unfold, the central thesis of personalized medicine—that treatment should be tailored to individual variation rather than population averages—will continue to transform both clinical evidence and practice.
The reliance on statistical significance, typically represented by the P-value, has long dominated the interpretation of clinical research findings. However, a result can be statistically significant without holding any practical value for patient care. This guide explores the critical distinction between statistical significance and clinical relevance, providing researchers and drug development professionals with methodologies and frameworks to ensure their work translates into meaningful patient outcomes. By examining the limitations of P-values, the importance of effect size estimation, and the application of patient-centered metrics like the Minimum Clinically Important Difference (MCID), we present a pathway for designing studies and interpreting data that bridges the gap between population averages and individual patient needs.
Statistical significance, often determined by a P-value of less than 0.05, has traditionally been a gatekeeper for scientific discovery and publication in biomedical research [132]. A P-value indicates the probability of observing a result as extreme as the one obtained, assuming the null hypothesis is true—it does not measure the probability that the null hypothesis is correct, the size of an effect, or its clinical importance [133]. This fundamental misunderstanding has led to widespread overconfidence in results classified as "significant," often at the expense of practical relevance [133] [134].
The over-reliance on P-values has several negative consequences. It can lead to publication bias, where only studies with small P-values are published, potentially skewing the evidence base [133]. Furthermore, the focus on achieving a P-value <0.05 has prompted practices like P-hacking, where data are manipulated or analyzed in multiple ways to achieve significance [133]. Perhaps most critically, this over-reliance distracts from the primary goal of medical research: to improve patient outcomes. A statistically significant result does not automatically mean the finding is clinically important [132] [135]. For drug development professionals, this distinction is paramount, as it influences decisions about which therapies warrant further investment and development.
Statistical Significance vs. Clinical Relevance: Fundamental Concepts
Defining the Terms
- Statistical Significance: This is a mathematical measure that helps determine whether an observed effect is likely due to chance. It is typically assessed through hypothesis testing, where a P-value < 0.05 leads to rejecting the null hypothesis. It answers the question, "Is there an effect?" [132] [134]
- Clinical Relevance (or Clinical Significance): This focuses on the practical importance of a finding in real-world contexts. It assesses whether an observed effect is meaningful enough to change patient management or improve patient outcomes, such as quality of life, survival, or symptom burden [132] [135]. It answers the question, "Does this effect matter to the patient?"
Key Differences and Potential Misalignments
The relationship between these two concepts is not always harmonious. Table 1 outlines common scenarios that researchers may encounter.
Table 1: Scenarios of Statistical vs. Clinical Significance
| Scenario | Statistical Significance | Clinical Relevance | Interpretation & Implication |
|---|---|---|---|
| Ideal Outcome | Yes | Yes | The finding is both unlikely to be due to chance and meaningful for patient care. Strong candidate for changing practice. |
| Dangerous Illusion | Yes | No | The effect is detectable (often due to large sample size) but too small to benefit patients. Risk of adopting useless treatments. |
| Missed Opportunity | No | Yes | The effect is meaningful but not statistically detectable (e.g., due to small sample size). May warrant further study in a larger trial. |
| Null Finding | No | No | The intervention does not demonstrate a detectable or meaningful effect. |
A classic example of the "Dangerous Illusion" is a study evaluating a new analgesic that reports a statistically significant reduction in pain scores (P=0.03) but where the absolute reduction is only 1 point on a 10-point scale. If the established MCID for pain relief is 2 points, this statistically significant result is not clinically relevant, and the treatment should not be considered sufficiently effective [133].
Key Statistical Metrics Beyond the P-Value
To bridge the gap between statistical significance and clinical meaning, researchers must incorporate additional metrics into their study design and reporting.
Effect Size and Confidence Intervals
The effect size quantifies the magnitude of a treatment effect, independent of sample size. Unlike the P-value, it provides a direct measure of whether an effect is large enough to be of practical concern [132]. Confidence Intervals (CIs) complement effect sizes by providing a range of plausible values for the true population effect. A 95% CI that excludes the null value (e.g., 0 for a difference in means) indicates statistical significance at the 5% level. More importantly, examining where the entire CI lies in relation to a clinically important threshold offers a richer interpretation than a P-value alone [133] [120].
The Minimum Clinically Important Difference (MCID)
The MCID is defined as the smallest change in an outcome that patients perceive as beneficial and which would lead to a change in patient management [133]. It provides a patient-centered benchmark against which to judge study results.
Application in Research:
- Study Design: Using the MCID in sample size calculations ensures studies are powered to detect clinically meaningful differences, not just statistically significant ones [133].
- Interpretation: Findings should be interpreted by comparing the effect size and its CI to the pre-specified MCID. An effect can be statistically significant but fail to meet the MCID, rendering it clinically irrelevant [133].
Alternative Statistical Approaches
- Bayesian Methods: These allow for the incorporation of prior evidence or belief into the analysis, and can provide more intuitive probabilistic statements about treatment effects (e.g., "There is a 95% probability that the treatment improves outcomes by at least the MCID") [133].
- Second-Generation P-Values (SGPV): This approach accounts for effect size and uncertainty by measuring how much a confidence interval overlaps a null region representing trivial effect sizes. It provides more nuanced conclusions about the support for meaningful effects [133].
Methodologies for Comparing Population Means with Clinical Relevance
The comparison of two independent population means is a common task in clinical trials. The following protocol details how to conduct and interpret such a test with a focus on clinical relevance.
Experimental Protocol: Aspin-Welch t-Test for Independent Samples
This test is used when comparing the means of two independent groups (e.g., treatment vs. control) with unknown and possibly unequal population standard deviations [118] [119].
1. Hypothesis Formation:
- Null Hypothesis (H₀): μ₁ = μ₂ (The population means are equal.)
- Alternative Hypothesis (Hₐ): Can be two-tailed (μ₁ ≠ μ₂), left-tailed (μ₁ < μ₂), or right-tailed (μ₁ > μ₂).
2. Data Collection:
- Obtain two independent simple random samples from the populations of interest.
- For each sample, calculate the sample mean (( \bar{x} )), sample standard deviation (s), and sample size (n).
3. Test Statistic Calculation: The test statistic is a t-score calculated as follows: [ t = \frac{(\bar{x}1 - \bar{x}2) - (\mu1 - \mu2)}{\sqrt{\frac{s1^2}{n1} + \frac{s2^2}{n2}}} ] In the context of testing the null hypothesis, (μ₁ - μ₂) is typically set to 0 [118] [119]. The denominator, (\sqrt{\frac{s1^2}{n1} + \frac{s2^2}{n2}}), is the standard error of the difference in means [120].
4. Degrees of Freedom (df) Calculation: The df for the Aspin-Welch test is calculated using a specific formula. In practice, this is computed using statistical software [119]: [ df = \frac{\left( \frac{s1^2}{n1} + \frac{s2^2}{n2} \right)^2}{\frac{1}{n1-1}\left( \frac{s1^2}{n1} \right)^2 + \frac{1}{n2-1}\left( \frac{s2^2}{n2} \right)^2} ]
5. Decision Making: Compare the calculated t-score to the critical t-value from the Student's t-distribution with the calculated df, or compare the P-value to the significance level (α, usually 0.05). If p ≤ α, reject the null hypothesis.
Workflow for Integrating Clinical Relevance into Data Analysis
The following diagram illustrates a robust workflow for analyzing and interpreting clinical trial data that prioritizes clinical relevance.
The Researcher's Toolkit: Essential Reagents for Robust Inference
Table 2: Key Analytical "Reagents" for Clinical Research
| Tool | Primary Function | Role in Bridging the Gap |
|---|---|---|
| MCID Definition | Establishes a patient-centered threshold for meaningfulness. | Shifts the focus from "is there an effect?" to "is the effect large enough to matter?" [133]. |
| Effect Size Calculator | Quantifies the magnitude of the treatment effect (e.g., Cohen's d). | Provides a scale-invariant measure of impact that is more informative than a P-value [132]. |
| Confidence Interval Interpreter | Estimates a range of plausible values for the true population effect. | Allows researchers to see if the entire range of plausible effects is clinically meaningful or trivial [120]. |
| Power Analysis Software | Determines the sample size required to detect an effect of a given size. | Ensures studies are designed to be sensitive to clinically relevant differences (MCID), not just any statistically significant difference [133]. |
| Bayesian Analysis Package | Incorporates prior knowledge and provides probabilistic results. | Generates more intuitive outputs for decision-makers (e.g., probability of exceeding MCID) [133]. |
Moving from statistical significance to clinical meaningfulness requires a fundamental shift in how clinical research is designed, analyzed, and interpreted. The exclusive reliance on P-values is an inadequate strategy for determining the value of a therapeutic intervention. By adopting a framework that prioritizes the Minimum Clinically Important Difference, rigorously reporting effect sizes and confidence intervals, and considering real-world factors like cost and generalizability, researchers and drug developers can ensure their work genuinely addresses the needs of individual patients.
The future of meaningful clinical research lies in embracing this multi-dimensional approach to evidence, moving beyond the simplistic dichotomy of "significant" or "not significant" to a more nuanced and patient-centered interpretation of what makes a finding truly matter.
Conclusion
The journey from population averages to individual patient care is both a fundamental challenge and the cornerstone of precision medicine. This synthesis demonstrates that ignoring individual variation risks ineffective or unsafe treatments for substantial patient subgroups, while embracing it through advanced methodologies like population PK, mixed-effects modeling, and replicated designs unlocks true personalization. The future of biomedical research lies in moving beyond the 'average' as a sufficient guide and instead building a robust evidence base that acknowledges and investigates the full spectrum of human diversity. This will require a concerted shift toward collecting richer datasets, adopting more sophisticated analytical techniques, and validating frameworks that prioritize predictiveness for the individual, ultimately ensuring that no patient is treated as merely 'average'.
References
- 1. When Averages Hide Individual Differences in Clinical Trials [https://www.americanscientist.org/article/when-averages-hide-individual-differences-in-clinical-trials]
- 2. Understanding statistical populations and inferences [https://www.sciencedirect.com/science/article/pii/S0028377024000791]
- 3. 3.2 Samples Versus Populations - BSCI 1510L Literature and ... [https://researchguides.library.vanderbilt.edu/c.php?g=69346&p=832048]
- 4. About Research: Clinical Versus Statistical Significance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11992633/]
- 5. Distinguishing Clinical from Statistical Significances in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11087199/]
- 6. The difference between statistical significance and clinical ... [https://www.sciencedirect.com/science/article/pii/S0020138323003935]
- 7. Population Pharmacokinetic/Pharmacodynamic Model ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2018.01316/full]
- 8. variance components and personalised medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5054923/]
- 9. Mastering Variability in Drug Response [https://select-statistics.co.uk/news/mastering-variability-in-drug-response/]
- 10. Quantitative Research Techniques for Drug Development [https://esr-research.com/quantitative-research-techniques-for-drug-development-surveys-and-statistical-analysis/]
- 11. Investigating variability in patient response to treatment [https://www.ovid.com/journals/smmr/pdf/10.1177/0962280210379174~investigating-variability-in-patient-response-to-treatment--]
- 12. A variance-ratio meta-analysis and estimation of treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S0887618522000846]
- 13. Statistical methods for assessing drug interactions using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10810670/]
- 14. Heterogeneous treatment effects and homogeneous ... [https://rpsychologist.com/hte-variance-ratio/]
- 15. Prevalence of actionable pharmacogenetic variants and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11391267/]
- 16. Cataloging Actionable Pharmacogenomic Variants for ... [https://www.mdpi.com/2039-4713/15/4/101]
- 17. Targeted adaptive sampling enables clinical ... [https://www.nature.com/articles/s41598-025-22941-z]
- 18. The global spectrum of protein-coding pharmacogenomic diversity [https://www.nature.com/articles/tpj201677?error=cookies_not_supported&code=33ced94c-8b98-4648-82b9-4dfbaaaabfd5]
- 19. Pharmacogenomic Testing: Clinical Evidence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789586/]
- 20. for Health Equity - PMC Population Pharmacogenomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC10606908/]
- 21. Identification and functional validation of novel ... [https://www.sciencedirect.com/science/article/abs/pii/S1043661822000329]
- 22. Dynamic star allele definitions in Pharmacogenomics [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1584658/full]
- 23. CYP2D6 pharmacogenomics [https://www.sciencedirect.com/science/article/pii/S1110863017300228]
- 24. CYP2D6 Overview: Allele and Phenotype Frequencies - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK574601/]
- 25. Atomoxetine: A Review of Its Pharmacokinetics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4876529/]
- 26. Individualized atomoxetine response and tolerability in ... [https://www.nature.com/articles/s41398-024-02859-2]
- 27. Dopamine Transporter and CYP2D6 Gene Relationships with ... [https://pubmed.ncbi.nlm.nih.gov/39387268/]
- 28. Basic Concepts in Population Modeling, Simulation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3606044/]
- 29. Population pharmacokinetics: an overview [https://australianprescriber.tg.org.au/articles/population-pharmacokinetics-an-overview.html]
- 30. Clinical Pharmacogenetics Implementation Consortium ... [https://pubmed.ncbi.nlm.nih.gov/30801677/]
- 31. CPIC® Guideline for Atomoxetine based on CYP2D6 ... [https://cpicpgx.org/guidelines/cpic-guideline-for-atomoxetine-based-on-cyp2d6-genotype/]
- 32. Informing the Treatment of Individual Patients Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6777993/]
- 33. Aging and aging-related diseases: from molecular ... [https://www.nature.com/articles/s41392-022-01251-0]
- 34. Molecular mechanisms of aging and anti-aging strategies [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01663-1]
- 35. Influence of Ageing on the Pharmacodynamics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11954733/]
- 36. Insights from Elderly Cohort Using g-Nomic® Software - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11123674/]
- 37. Lifestyles and their relative contribution to biological aging ... [https://elifesciences.org/articles/99924]
- 38. Population PK for the Physician Scientist [https://www.rxmd.com/population-pk-for-the-physician-scientist/]
- 39. Population Pharmacokinetic Method to Predict Within ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7913178/]
- 40. Blog | Diversity in Preclinical Research [https://insphero.com/diversity-in-preclinical-research/]
- 41. Bioequivalence [https://onlinehelp.certara.com/phoenix/8.2/topics/bioeqoverview.htm]
- 42. What is the Difference Between Individual and Population ... [https://www.certara.com/knowledge-base/what-is-the-difference-between-individual-and-population-pk/]
- 43. What Is Population Pharmacokinetic (popPK) Analysis? [https://www.allucent.com/resources/blog/what-population-pharmacokinetic-poppk-analysis]
- 44. Population PK (PopPK): The What, The How, and The Why [https://www.quantics.co.uk/blog/poppk-the-what-the-how-and-the-why/]
- 45. Introduction to Pharmacokinetic Modeling Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636497/]
- 46. Population pharmacokinetics/pharmacodynamics analysis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1631034/full]
- 47. Population Pharmacokinetic Model Evaluation with a Small ... [https://pubmed.ncbi.nlm.nih.gov/40730936/]
- 48. Comparing Scientific Machine Learning With Population ... [https://pubmed.ncbi.nlm.nih.gov/39921335/]
- 49. A machine learning approach to population ... [https://www.nature.com/articles/s43856-025-01054-8]
- 50. A comparison of two sparse sampling population ... [https://pubmed.ncbi.nlm.nih.gov/15124982/]
- 51. A Post Hoc Analysis of a Pharmacokinetic Study ... [https://www.sciencedirect.com/science/article/abs/pii/S0149291812000690]
- 52. Reporting guidelines for population pharmacokinetic analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC4432104/]
- 53. An automated pipeline to generate initial estimates for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592298/]
- 54. An automated classification pipeline for tables in ... [https://www.nature.com/articles/s41598-025-94778-5]
- 55. A brief introduction to mixed effects modelling and multi-model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5970551/]
- 56. Apportioning Variation in Multilevel Models - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK565709/]
- 57. When to use mixed effect model? - Cross Validated [https://stats.stackexchange.com/questions/275450/when-to-use-mixed-effect-model]
- 58. Nonlinear mixed-effects models for modeling in vitro drug ... [https://www.nature.com/articles/s41598-019-50936-0]
- 59. variancePartition: interpreting drivers of variation in complex ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-016-1323-z]
- 60. Multi-Level Modeling [https://www.publichealth.columbia.edu/research/population-health-methods/multi-level-modeling]
- 61. Optimizing Aggregated N-Of-1 Trial Designs for Predictive ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2020.00013/full]
- 62. Comparison of Aggregated N-of-1 Trials with Parallel and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6955665/]
- 63. An Introduction to the Cross-Over Trial Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11534298/]
- 64. A Comparison of Four Methods for the Analysis of N-of-1 Trials [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0087752]
- 65. A methodological review of randomised n-of-1 trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11020886/]
- 66. Comparison of Aggregated N-of-1 Trials with Parallel and ... [https://pubmed.ncbi.nlm.nih.gov/31698799/]
- 67. Design, analysis, and presentation of crossover trials [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-10-27]
- 68. A framework for N-of-1 trials of individualized gene ... [https://www.nature.com/articles/s41467-024-54077-5]
- 69. Understanding Population, Sample, and Measures of Data ... [https://medium.com/@saurabhkothawade01/understanding-population-sample-and-measures-of-data-variability-in-machine-learning-12b97f79f09b]
- 70. Advancements in Predicting Human Life Outcomes - Simple Science [https://scisimple.com/en/articles/2025-10-30-advancements-in-predicting-human-life-outcomes--a3dp182]
- 71. Mining big to extract patterns and data real-life predict . outcomes [https://colab.ws/articles/10.1037%2Fmet0000105]
- 72. What Is Predictive ? | IBM AI [https://www.ibm.com/think/topics/predictive-ai]
- 73. Enhancing Patient Outcome Prediction Through Deep ... [https://www.jmir.org/2025/1/e57358]
- 74. Model validation in machine learning: How to do it [https://www.leewayhertz.com/model-validation-in-machine-learning/]
- 75. Top 5 Validation Methods In Machine Learning [https://medium.com/@mehmetalitor/top-5-model-validation-methods-in-machine-learning-77eed8d08937]
- 76. While AI Could Be the Game Changer in Predicting Health ... [https://www.medschool.umaryland.edu/news/2025/while-ai-could-be-the-game-changer-in-predicting-health-outcomes-it-should-not-be-the-only-method.html]
- 77. Parsing interindividual drug variability: an emerging role for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4696409/]
- 78. Of Mice and Men: The Inter-individual Variability ... [https://www.eneuro.org/content/11/2/ENEURO.0518-23.2024]
- 79. Exposure-Response Modeling to Support Dosing Selection ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.645130/full]
- 80. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 81. PHARMACOMETRIC APPROACHES TO IMPROVING ... [https://hammer.purdue.edu/articles/thesis/_b_PHARMACOMETRIC_APPROACHES_TO_IMPROVING_MEDICATION_SAFETY_AND_EFFICACY_b_/29691557]
- 82. Simpson's paradox [https://en.wikipedia.org/wiki/Simpson%27s_paradox]
- 83. Simpson's Paradox: When Aggregated Data Tells a ... [https://www.statology.org/simpsons-paradox-when-aggregated-data-tells-a-different-story/]
- 84. Simpson's Paradox - Stanford Encyclopedia of Philosophy [https://plato.stanford.edu/entries/paradox-simpson/]
- 85. 21.2 Simpson's Paradox | A Guide on Data Analysis [https://bookdown.org/mike/data_analysis/simpsons-paradox.html]
- 86. diversity in oncology Population responses and implications to... drug [https://cco.amegroups.org/article/view/26234/html]
- 87. The Population Approach: Rationale, Methods, and... | SpringerLink [https://link.springer.com/chapter/10.1007/978-3-642-78680-8_15]
- 88. Understanding Individual in Variations Responses: From... Drug [https://www.nigms.nih.gov/News/meetings/Pages/DrugResponses]
- 89. Simpson's Paradox Explained [https://www.statsig.com/perspectives/simpsons-paradox-explained]
- 90. The benefits of single-subject research designs and multi-methodological approaches for neuroscience research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10634204/]
- 91. 10.1 Overview of Single-Subject Research [https://opentext.wsu.edu/carriecuttler/chapter/overview-of-single-subject-research/]
- 92. Single-Subject Experimental Design: An Overview [https://tlr-hub.asha.org/conducting-and-reporting-of-research/single-subject-experimental-design-an-overview-2/]
- 93. Single-Subject Experimental Design for Evidence-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3992321/]
- 94. Single Subject Research [https://researchbasics.education.uconn.edu/single-subject-research/]
- 95. Single-case experimental designs to assess intervention ... [https://www.sciencedirect.com/science/article/pii/S1877065717304542]
- 96. A reference set of clinically relevant adverse drug- ... [https://www.nature.com/articles/s41597-022-01159-y]
- 97. Clinical relevance and methodological approach for the ... [https://www.sciencedirect.com/science/article/pii/S2059702925009883]
- 98. Study Design and Analysis for Assessment of Interactions - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK19921/]
- 99. Within, among, or between? [http://ecoevoevoeco.blogspot.com/2022/12/within-among-or-between.html]
- 100. Power Determination During Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC6430154/]
- 101. Design and statistics of pharmacokinetic drug-drug, herb ... [https://www.sciencedirect.com/science/article/pii/S0753332223006133]
- 102. Optimizing drug development: strategies to assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2014497/]
- 103. Variance reduction in experiments using covariate ... [https://medium.com/glovo-engineering/variance-reduction-in-experiments-using-covariate-adjustment-techniques-717b1e450185]
- 104. When does adjusting covariate under randomization help? A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11514882/]
- 105. Unlocking 66% Faster Experiments with Covariate ... [https://tech.instacart.com/unlocking-66-faster-experiments-with-covariate-adjustment-power-analysis-for-clustered-data-3a0c11c7baa6]
- 106. Variance reduction combining pre-experiment and in- ... [https://arxiv.org/html/2410.09027v1]
- 107. Covariate modeling in pharmacometrics: General points for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11098153/]
- 108. Covariate selection in pharmacometric analyses: a review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4294083/]
- 109. What is Bioequivalence? [https://www.quantics.co.uk/blog/what-is-bioequivalence/]
- 110. ABE IBE PBE | PPT [https://www.slideshare.net/slideshow/abe-ibe-pbe/14479828]
- 111. Bioequivalence Data Analysis [https://docs.pumas.ai/dev/bioequivalence/be_analysis/]
- 112. Bioavailability and Bioequivalence in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4157693/]
- 113. The Reference-scaled Average Bioequivalence (RSABE) ... [https://www.certara.com/blog/reference-scaled-average-bioequivalence-2/]
- 114. and four-period crossover studies [https://www.sciencedirect.com/science/article/abs/pii/S0169260702000196]
- 115. Reference-Scaled Average Bioequivalence - An Introduction [https://www.linkedin.com/pulse/reference-scaled-average-bioequivalence-introduction-chandramouli-r-bbuvc]
- 116. Between-Batch Bioequivalence (BBE): a Statistical Test to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7651657/]
- 117. NASAL SPRAY BIOEQUIVALENCE - Between-Batch ... [https://drug-dev.com/nasal-spray-bioequivalence-between-batch-bioequivalence-bbe-an-alternative-statistical-method-to-assess-in-vitro-bioequivalence-of-nasal-product/]
- 118. 7.7: Comparing Two Independent Population Means [https://stats.libretexts.org/Courses/Saint_Mary's_College_Notre_Dame/BFE_1201_Statistical_Methods_for_Finance_(Kuter)/07%3A_Hypothesis_Testing/7.07%3A_Comparing_Two_Independent_Population_Means]
- 119. Testing for Two Population Means [https://courses.lumenlearning.com/introstatscorequisite/chapter/two-population-means-with-unknown-standard-deviations/]
- 120. Estimating the Difference in Two Population Means [https://pressbooks.cuny.edu/conceptsinstatistics/chapter/estimating-the-difference-in-two-population-means/]
- 121. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 122. FDA Advances Rare Disease Drug Development with New ... [https://www.fda.gov/news-events/press-announcements/fda-advances-rare-disease-drug-development-new-evidence-principles]
- 123. A Benchmark, Expand, and Calibration (BenchExCal) Trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087693/]
- 124. The limitations of evidence-based medicine compel ... [https://link.springer.com/article/10.1007/s00134-024-07528-y]
- 125. Understanding Individual Subject Differences through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11035513/]
- 126. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 127. Application of a Personalised Approach in Clinical Practice [https://jpmsonline.com/article/individualised-medicine-application-of-a-personalised-approach-in-clinical-practice-750/]
- 128. The Rise of Personalized Medicine in 2025 [https://vasro.de/en/pharmaceutical-biotechnology-trends-2025/]
- 129. 10.2: Comparing Two Independent Population Means [https://stats.libretexts.org/Courses/Fresno_City_College/Book%3A_Business_Statistics_Customized_(OpenStax)/10%3A_Hypothesis_Testing_with_Two_Samples/10.02%3A_Comparing_Two_Independent_Population_Means]
- 130. Treatment Personalization and Precision Mental Health Care [https://pmc.ncbi.nlm.nih.gov/articles/PMC11379769/]
- 131. Precision Medicine Trends 2025: Top 6 Powerful Positive ... [https://lifebit.ai/blog/precision-medicine-trends-2025/]
- 132. Statistical Significance versus Clinical Relevance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11633268/]
- 133. why statistical significance is not enough in clinical practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947593/]
- 134. Statistical significance or clinical significance? A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8477766/]
- 135. Clinical Relevance and Statistical Significance. How can ... [https://www.rgnmed.com/post/clinical-relevance-and-statistical-significance-how-can-we-achieve-both-using-real-world-data]