Experimental vs. Observational Studies: A Researcher's Guide to Design, Application, and Evidence-Based Decision Making
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the critical distinction between experimental and observational studies.
Experimental vs. Observational Studies: A Researcher's Guide to Design, Application, and Evidence-Based Decision Making
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the critical distinction between experimental and observational studies. It covers the foundational definitions and core characteristics of each methodology, details their specific applications and design implementations, addresses common challenges and optimization strategies, and offers a framework for the critical evaluation and comparison of evidence. By synthesizing these four intents, the article empowers professionals to select the most rigorous and appropriate study design for their research questions, ultimately strengthening the validity and impact of biomedical and clinical research.
Laying the Groundwork: Core Principles of Experimental and Observational Research Designs
In the rigorous world of scientific research, particularly in drug development and clinical trials, the choice of study design is foundational. The path to generating evidence—whether for a new therapeutic compound or an understanding of disease progression—is largely dictated by two primary methodological paradigms: experimental and observational studies. The former is characterized by active intervention and researcher-controlled manipulation of variables, while the latter involves passive observation of subjects in their natural state without any intervention [1] [2]. Within the context of clinical research, both designs significantly contribute to the advancement of medical knowledge, enabling scientists to develop effective new treatments and improve patient care [2]. This guide provides an objective comparison of these two approaches, detailing their defining protocols, applications, and the distinct types of data they yield.
Core Definitions and Methodologies
What is an Experimental Study?
An experimental study is a research design wherein an investigator deliberately manipulates one or more independent variables to establish a cause-effect relationship with a dependent variable [1]. This design is defined by the high degree of control exerted by the researcher and is often used to test specific, predictive hypotheses.
The quintessential example of an experimental study in clinical research is the Randomized Controlled Trial (RCT) [2]. In an RCT, participants are randomly assigned to either an experimental group, which receives the new intervention (e.g., a drug), or a control group, which receives a placebo or standard treatment. This randomization minimizes selection bias and ensures that the groups are comparable, making it the gold standard for establishing the efficacy and safety of new medical interventions [2].
Detailed Experimental Protocol (RCT):
- Hypothesis Formulation: The researcher defines a predictive statement (e.g., "New Drug A lowers blood pressure more effectively than the current standard treatment").
- Participant Recruitment and Randomization: A sample of the target population is recruited. Participants are then randomly allocated, often using computer-generated sequences, to either the experimental or control group. This process ensures that every participant has an equal chance of being in either group, reducing the influence of confounding variables [1].
- Blinding (Masking): In a single-blind study, participants are unaware of their group assignment. In a double-blind study, neither the participants nor the researchers administering the treatment know which group is which. This prevents bias in the reporting and assessment of outcomes [2].
- Intervention and Control: The experimental group receives the intervention under investigation, while the control group receives a placebo or an established alternative.
- Data Collection and Follow-up: Data on the dependent variable(s) (e.g., blood pressure readings) are collected from both groups over a specified period.
- Data Analysis: Statistical analyses are performed to compare outcomes between the groups and determine if observed differences are statistically significant.
What is an Observational Study?
An observational study is a non-experimental research method in which the researcher merely observes subjects and measures variables of interest without interfering or manipulating any variables [1] [2]. The goal is to capture naturally occurring behaviors, conditions, or events, and the data collected often reflect real-world situations.
Observational studies are not a single entity but are categorized into specific types based on their design [2]:
- Cohort Studies: These follow a group of people (a cohort) over a period of time. They can be prospective (following participants forward in time) or retrospective (looking back at historical data). For example, a study might observe a large group of individuals without heart disease to see who develops it, comparing those who smoke and those who do not.
- Case-Control Studies: These compare a group of individuals with a specific disease or condition (the "cases") to a similar group without that condition (the "controls"). Researchers then look back to identify differences in exposure or behavior between the two groups.
- Cross-Sectional Studies: These gather data from a cross-section of the population at a single point in time, typically through surveys or interviews, to assess the prevalence of a disease or condition.
Detailed Observational Protocol (Prospective Cohort Study):
- Research Question Definition: The researcher defines a question about the relationship between an exposure and an outcome (e.g., "Does a sedentary lifestyle increase the risk of developing type 2 diabetes?").
- Cohort Selection and Group Assignment: A sample is selected, often based on certain characteristics. Crucially, participants are not assigned to groups by the researcher; instead, they are grouped based on their naturally occurring exposure status (e.g., sedentary vs. active lifestyle) [2].
- Observation and Data Collection: Researchers collect data on exposures, confounders (e.g., age, diet), and outcomes over time without intervening. This is often done through medical records, surveys, or direct measurements in natural settings.
- Follow-up: The cohort is followed for a period to track the incidence of the outcome of interest.
- Data Analysis: Statistical models are used to analyze the association between the exposure and the outcome, while attempting to control for identified confounding variables.
Direct Comparison: Experimental vs. Observational Studies
The table below summarizes the key differences, strengths, and weaknesses of these two research paradigms.
| Aspect | Experimental Study | Observational Study |
|---|---|---|
| Core Objective | To determine cause-and-effect relationships [1] | To explore associations and correlations between variables [1] |
| Variable Manipulation | Direct manipulation of independent variables by the researcher [1] | No manipulation; variables are measured as they naturally occur [1] |
| Control & Bias | High level of control reduces confounding variables; random assignment minimizes selection bias [1] [2] | Low level of control; susceptible to confounding variables and selection bias [1] [2] |
| Establishing Causality | Able to establish causality [1] | Cannot establish causality, only correlation [1] |
| Generalizability | Sometimes limited due to controlled, artificial conditions and strict eligibility criteria (lack of ecological validity) [1] [2] | Higher ecological validity, as observations are made in real-world settings; however, findings may not apply to broader populations [1] [2] |
| Ethical Considerations | Ethical constraints exist for manipulations that could harm subjects (e.g., testing a known harmful substance) [1] [2] | Ethical method for studying harmful exposures or when manipulation is impractical (e.g., studying the effects of smoking) [2] |
| Time & Cost | Often time-consuming and costly due to need for strict controls and monitoring [1] [2] | Generally less time-consuming and costly, though long-term cohort studies can be expensive [1] |
| Primary Strengths | Establishes causality; high internal validity; results are replicable [1] [2] | Studies phenomena unethical or impractical to manipulate; high external/ecological validity [1] [2] |
| Primary Weaknesses | Potential for artificiality; ethical limitations; can be expensive [1] [2] | Cannot prove causation; prone to various biases (confounding, recall, measurement) [1] [2] |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and solutions used across clinical research studies, with their specific functions in both experimental and observational contexts.
| Item | Function in Research |
|---|---|
| Placebo | An inert substance identical in appearance to the active drug; administered to the control group in an RCT to blind participants and researchers, isolating the specific effect of the intervention from psychological effects [2]. |
| Data Collection Tools (e.g., Surveys, CRFs) | Standardized forms (Case Report Forms in trials, surveys in observational studies) used to systematically collect participant data on exposures, outcomes, and potential confounders, ensuring consistency and completeness [2] [3]. |
| Blinding Protocol | A methodological procedure (single or double-blind) where information about the intervention is concealed from participants and/or researchers to prevent bias in outcome assessment and reporting [2]. |
| Randomization Schedule | A computer-generated sequence or other formal plan used to randomly assign eligible participants to study groups, ensuring each has an equal chance of assignment to any group, thereby minimizing selection bias [1] [2]. |
| Statistical Analysis Software (e.g., R, SAS, SPSS) | Software packages (R, Python, SPSS, SAS) used to perform descriptive and inferential statistical analyses, from calculating p-values and confidence intervals to running complex regression models [3]. |
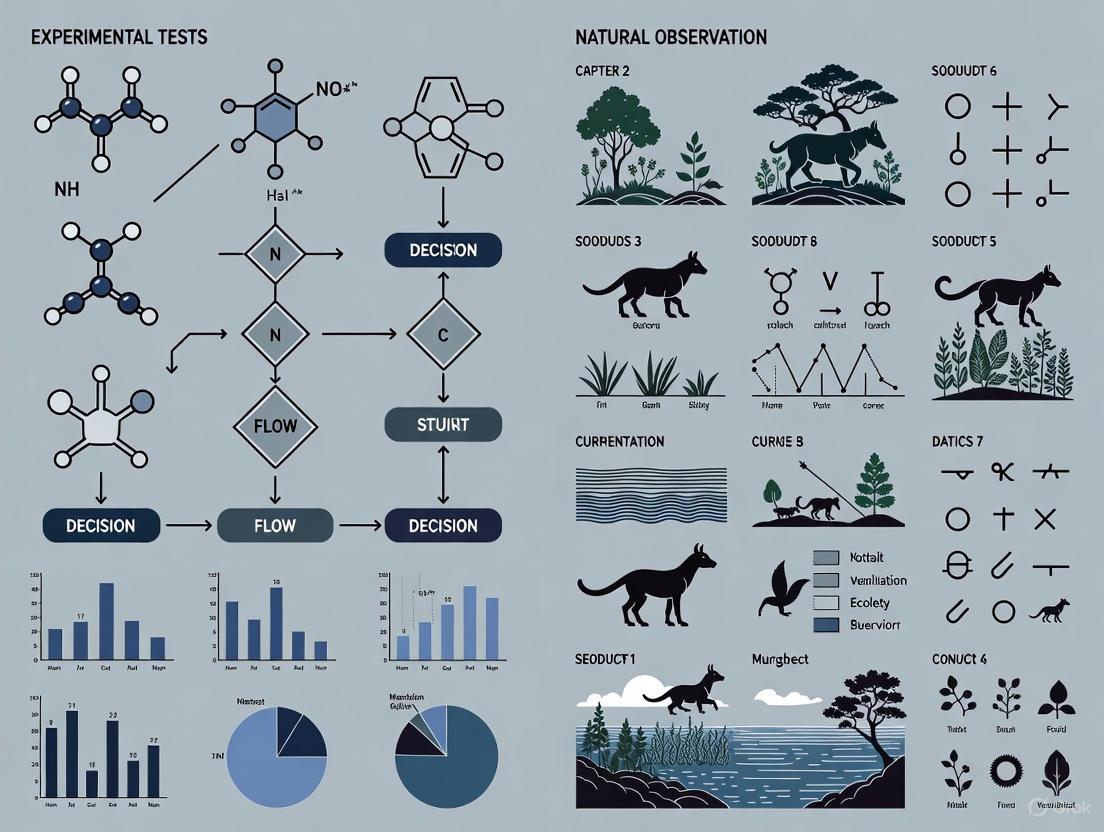
Visualizing Research Design Workflows
The logical pathways for conducting experimental and observational studies are fundamentally different. The diagrams below, created using the specified color palette, illustrate these distinct workflows.
Experimental Study Workflow (Randomized Controlled Trial)
Observational Study Workflow (Prospective Cohort)
Experimental and observational studies are complementary pillars of clinical research. The controlled, interventional nature of experimental studies like RCTs makes them the definitive method for establishing causal efficacy and bringing new drugs to market. In contrast, observational studies provide indispensable real-world evidence on long-term outcomes, effectiveness in diverse populations, and the risks and benefits of interventions as used in clinical practice. A robust research strategy understands the strengths and limitations of each paradigm, leveraging them appropriately to build a comprehensive body of evidence that ultimately advances scientific knowledge and improves patient care.
Manipulation, Control, Randomization, and Natural Setting
In scientific research, the choice between experimental tests and natural observation is fundamental, shaping the methodology, validity, and applicability of the findings. Experimental studies are characterized by active manipulation of variables and controlled conditions, whereas natural observation involves examining subjects in their native environments without intervention. This guide provides a detailed comparison of these approaches, focusing on the core characteristics of manipulation, control, randomization, and natural setting, to aid researchers, scientists, and drug development professionals in selecting the appropriate design for their investigative goals.
Core Characteristics Comparison
The table below summarizes the key differences between experimental and observational studies across the defining features of research design.
| Characteristic | Experimental Studies | Observational Studies (Natural Observation) |
|---|---|---|
| Manipulation | Active intervention by the researcher; the independent variable is manipulated. [4] | No intervention; variables are studied as they naturally occur. [4] |
| Control | High level of control over the environment and variables to isolate cause and effect. [4] | Minimal to no control; the setting is observed without alteration. [4] |
| Randomization | Random assignment of participants to control and experimental groups is a key feature. [5] [4] | Typically, no random assignment; participants are observed in pre-existing groups. [4] |
| Setting | Often conducted in controlled laboratory settings. [4] | Conducted in natural, real-world settings. [4] |
| Ability to Establish Causation | Strong, considered the "gold standard" for establishing cause-and-effect relationships. [5] [4] | Limited; can identify associations and correlations but not definitive causation. [4] |
| Susceptibility to Confounding Factors | Low, as control and randomization minimize the impact of confounding variables. [4] | High, due to the inability to control for all external factors that may influence outcomes. [4] |
| Ethical Considerations | May be unethical or impractical when manipulation could cause harm. [4] | Often preferred when it is unethical to manipulate variables or assign participants to groups. [4] |
Detailed Methodological Protocols
Experimental Study Protocol: Randomized Controlled Trial (RCT)
The RCT is the quintessential experimental design for establishing causal inference, particularly in clinical trials and drug development [5] [4].
- Objective: To determine the causal effect of a new drug (Intervention X) on blood pressure compared to a standard treatment.
- Key Methodological Steps:
- Hypothesis Formulation: State a specific, testable hypothesis (e.g., "Intervention X reduces systolic blood pressure more effectively than the standard treatment").
- Participant Recruitment and Randomization: Recruit eligible participants and use a computer-generated sequence to randomly assign them to either the intervention group (receives Intervention X) or the control group (receives the standard treatment or a placebo). This process helps ensure groups are comparable at baseline. [5] [4]
- Blinding: Implement single- (participants unaware) or double-blinding (participants and researchers unaware) to prevent bias.
- Intervention and Control: Administer the designated treatment to each group under strictly controlled and monitored conditions. [4]
- Outcome Measurement: Measure the primary outcome (e.g., change in systolic blood pressure) at predefined time points for both groups.
- Data Analysis: Compare the outcomes between the intervention and control groups using statistical tests (e.g., t-tests) to determine if observed differences are statistically significant. [4]
Observational Study Protocol: Cohort Study
Cohort studies are a primary form of natural observation that follow a group of people over time to investigate the causes of disease [5].
- Objective: To explore the association between a specific occupational exposure (e.g., prolonged exposure to Chemical A) and the incidence of a rare lung disease.
- Key Methodological Steps:
- Cohort Definition: Identify and enroll a group of workers exposed to Chemical A and a comparable group of workers not exposed. [5]
- Natural Setting Observation: Follow both cohorts over a long period (often years) in their actual work and life environments, without any intervention by the researcher. [4]
- Data Collection: Periodically collect data on health outcomes, lifestyle factors, and other relevant variables through medical records, surveys, or health screenings.
- Control for Confounding: Use statistical techniques like multiple regression analysis to account for potential confounding variables (e.g., age, smoking status) that could influence the results. [6] [4]
- Outcome Analysis: Calculate and compare the incidence rates of the lung disease between the exposed and non-exposed cohorts to determine if an association exists. [5]
Research Workflow and Causal Inference Logic
The following diagram illustrates the high-level logical pathways and key decision points that differentiate experimental and observational research designs, culminating in their differing strengths for causal inference.
Essential Research Reagent Solutions
The table below details key materials and methodological components essential for conducting rigorous research in both experimental and observational contexts.
| Reagent/Methodological Component | Function in Research |
|---|---|
| Randomization Algorithm | A computational procedure for randomly assigning participants to study groups, which minimizes selection bias and distributes confounding factors evenly, thereby strengthening causal claims. [5] [4] |
| Control Group | A baseline group that does not receive the experimental intervention. It serves as a comparator to isolate and measure the true effect of the intervention by accounting for changes due to other factors. [4] |
| Blinding Protocol | A methodological procedure where participants (single-blind) and/or researchers and outcome assessors (double-blind) are kept unaware of group assignments to prevent conscious or unconscious bias that could influence the results. |
| Statistical Adjustment (e.g., Multiple Regression) | A suite of statistical techniques used primarily in observational studies to mathematically control for the influence of confounding variables, thereby providing a clearer picture of the relationship between the exposure and outcome of interest. [6] [4] |
| Standardized Data Collection Tool | Validated instruments such as surveys, medical imaging protocols, or laboratory assay kits that ensure consistent, reliable, and comparable measurement of variables across all participants in a study. [7] |
| Propensity Score Matching | An advanced statistical method used in quasi-experimental and observational studies to simulate randomization by matching each treated participant with one or more non-treated participants who have a similar probability (propensity) of receiving the treatment based on observed covariates. [6] |
Within the broader thesis of experimental tests versus natural observation research, the hierarchy of evidence provides a framework for ranking study designs based on their internal validity and ability to minimize bias. This guide objectively compares the two primary methodologies: Randomized Controlled Trials (RCTs), representing experimental tests, and Observational Studies, representing natural observation.
Comparative Performance: RCTs vs. Observational Studies
The following table summarizes quantitative data comparing the performance of RCTs and Observational Studies across key metrics.
Table 1: Quantitative Comparison of Study Designs
| Metric | Randomized Controlled Trial (RCT) | Cohort Study | Case-Control Study |
|---|---|---|---|
| Risk of Confounding Bias | Low (Theoretically 0 with perfect randomization) | Moderate to High | High |
| Ability to Establish Causality | High (Gold Standard) | Moderate | Low |
| Typical Sample Size | 100 - 10,000+ participants | 10,000 - 100,000+ participants | 500 - 5,000 participants |
| Relative Cost & Duration | High cost, Long duration | Moderate cost, Long duration | Lower cost, Shorter duration |
| Relative Risk (RR) / Odds Ratio (OR) Concordance with RCTs | Reference Standard | ~80% concordance for RR > 2 | ~70% concordance for OR > 4 |
| Ideal Use Case | Efficacy of a new drug or intervention | Long-term safety outcomes, rare exposures | Investigating rare diseases or outcomes |
Experimental Protocols
Protocol 1: Conducting a Parallel-Group Randomized Controlled Trial
- Protocol Development & Registration: A detailed study protocol is written, specifying objectives, design, endpoints, and statistical methods. It is registered on a public platform (e.g., ClinicalTrials.gov).
- Participant Screening & Recruitment: Eligible participants are identified based on strict inclusion/exclusion criteria.
- Informed Consent: All participants provide written, informed consent.
- Baseline Assessment & Randomization: Baseline data are collected. Participants are then randomly allocated to either the intervention group or the control group using a computer-generated sequence.
- Blinding (Masking): Participants, care providers, and outcome assessors are blinded to group assignment wherever possible.
- Intervention Period: The intervention group receives the investigational product (e.g., Drug A). The control group receives a placebo or standard-of-care treatment.
- Follow-up & Monitoring: Participants are followed for a predetermined period. Adherence, adverse events, and outcome data are systematically collected.
- Outcome Assessment: Primary and secondary endpoints (e.g., mortality, disease progression) are measured at the end of the study.
- Data Analysis: An intention-to-treat (ITT) analysis is typically performed to compare outcomes between the randomized groups.
Protocol 2: Conducting a Prospective Cohort Study
- Hypothesis Formulation: A hypothesis linking an exposure to an outcome is defined (e.g., "Does high sugar consumption lead to cardiovascular disease?").
- Cohort Assembly: A large group of participants, free of the outcome of interest, is recruited.
- Exposure Assessment: Participants are assessed and grouped based on their exposure status (e.g., high vs. low sugar diet) through questionnaires, biomarkers, or electronic health records. No intervention is applied by the researchers.
- Baseline Data Collection: Extensive data on potential confounders (e.g., age, sex, BMI, smoking status) are collected.
- Follow-up: The cohort is followed forward in time for a prolonged period (often years).
- Outcome Ascertainment: The occurrence of the outcome (e.g., heart attack) is identified through medical records, registries, or direct follow-up.
- Data Analysis: The incidence of the outcome in the exposed group is compared to the incidence in the unexposed group, calculating a Relative Risk (RR). Statistical adjustments (e.g., multivariate regression) are used to control for identified confounders.
Visualizing the Workflows and Hierarchy
Hierarchy of Evidence Pyramid
RCT Participant Workflow
Observational Study Design Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Clinical Research Studies
| Item | Function in Research |
|---|---|
| Investigational Product (IP) | The drug, device, or biologic being tested for efficacy and safety. |
| Placebo | An inert substance identical in appearance to the IP, used in the control arm to blind the study. |
| Randomization System | A computerized system or service that generates an unpredictable allocation sequence to assign participants to study groups. |
| Case Report Form (CRF) | A structured document (paper or electronic) for collecting all protocol-required data for each study participant. |
| Clinical Endpoint Adjudication Committee | An independent, blinded group of experts who review and validate potential outcome events, reducing measurement bias. |
| Biomarker Assay Kits | Standardized reagents (e.g., ELISA, PCR) to quantitatively measure biological molecules as indicators of exposure, disease, or treatment response. |
| Electronic Data Capture (EDC) System | A secure software platform for efficient and accurate collection of clinical trial data from investigational sites. |
| Statistical Analysis Software (SAS/R) | Programming environments used for complex statistical analyses, including regression modeling and handling of missing data. |
In scientific research, particularly in fields like drug development, the integrity of a study's conclusions hinges on a precise understanding of its core components. The relationship between independent variables (the presumed cause) and dependent variables (the presumed effect) forms the bedrock of experimental inquiry [8] [9]. Furthermore, the choice of research methodology—experimental tests versus natural observation—profoundly influences the degree to which causality can be inferred from these relationships [2] [1]. This guide provides an objective comparison of these two methodological approaches, detailing their protocols, strengths, and limitations to empower researchers in selecting the optimal design for their investigative goals.
An independent variable is the factor that the researcher manipulates, controls, or uses to group participants to test its effect on another variable [9]. Its value is independent of other variables in the study, making it the explanatory or predictor variable [8]. Conversely, a dependent variable is the outcome that researchers measure to see if it changes in response to the independent variable [9]. It "depends" on the independent variable and represents the effect or response in the cause-and-effect relationship being studied [8] [10]. Confounding variables are a critical third factor that can distort this relationship. These are extraneous variables that influence both the independent and dependent variables, potentially leading to incorrect conclusions about causality [11] [12].
Experimental Research vs. Natural Observation: A Comparative Analysis
The core distinction in research design lies in the researcher's level of control and intervention. The following table provides a structured comparison of these two primary approaches, summarizing their key characteristics, data presentation styles, and inherent challenges.
Table 1: Comparative Analysis of Experimental and Observational Research Designs
| Aspect | Experimental Research | Observational Research (Natural Observation) |
|---|---|---|
| Core Definition | A research method where the investigator actively manipulates one or more independent variables to establish a cause-and-effect relationship [2] [1]. | A non-experimental research method where the investigator observes subjects and measures variables without any interference or manipulation [2] [4]. |
| Researcher Control | High degree of control over the environment, variables, and participant assignment [1] [4]. | Minimal to no control; researchers observe variables as they naturally occur [2] [1]. |
| Primary Objective | To test specific hypotheses and definitively establish causation [1] [4]. | To identify patterns, correlations, and associations in real-world settings [2] [4]. |
| Ability to Establish Causality | High; the gold standard for inferring cause-and-effect due to manipulation and control of confounding factors [2] [1]. | Low; cannot establish causation, only correlation, due to the presence of uncontrolled confounding variables [1] [4]. |
| Key Methodological Features | - Manipulation of the independent variable- Random assignment of participants- Use of control groups [2] [1] | - No manipulation of variables- Observation in natural settings- Groups based on pre-existing characteristics [2] [4] |
| Data Presentation | Data is often presented to show differences between experimental and control groups, using measures like means and standard deviations. T-tests and ANOVAs are common analytical tests [8] [9]. | Data often shows associations between variables, presented as correlation coefficients or risk ratios. Regression analysis is frequently used to control for known confounders [11] [4]. |
| Common Challenges | - Can lack ecological validity (real-world applicability)- Ethical constraints on manipulations- Can be costly and time-consuming [2] [1] | - Highly susceptible to confounding variables- Potential for selection and observer bias- Cannot determine causality [2] [11] |
| Ideal Use Cases | - Establishing the efficacy of a new drug [2]- Testing a specific psychological intervention [9]- Studying short-term effects under controlled conditions [4] | - Studying long-term effects or rare events [2] [4]- When manipulation is unethical (e.g., smoking studies) [2] [1]- Large-scale population-based research [4] |
Visualizing Research Design and Confounding Variables
The logical flow of a research design and the insidious role of confounding variables can be effectively communicated through diagrams. The following workflows are generated using Graphviz DOT language, adhering to the specified color palette and contrast rules.
Experimental Research Workflow
The diagram below outlines the standard protocol for a true experimental design, such as a randomized controlled trial (RCT), which is central to establishing causality.
The Problem of Confounding Variables
This diagram illustrates how a confounding variable can create a false impression of a direct cause-and-effect relationship between the independent and dependent variables.
Detailed Experimental Protocols
Protocol for a Randomized Controlled Trial (RCT)
The RCT is the quintessential experimental design for establishing causality, especially in drug development [2]. The following protocol outlines its key phases.
Phase 1: Study Design and Preparation
- Hypothesis Formulation: Clearly state the predicted causal relationship. For example: "If patients with Condition X receive Drug Y (IV), then they will experience a greater reduction in Symptom Z (DV) compared to those receiving a placebo."
- Operationalization: Precisely define how the IV will be manipulated and the DV will be measured [9]. For instance, the IV is "10mg of Drug Y daily," and the DV is "the score on the Standardized Symptom Z Scale after 8 weeks."
- Participant Recruitment: Identify the target population using specific inclusion and exclusion criteria [2].
- Randomization: Use a computer-generated sequence to randomly assign eligible participants to either the experimental or control group. This is critical for minimizing selection bias and distributing known and unknown confounding variables evenly across groups [2] [1].
Phase 2: Intervention and Blinding
- Intervention: Administer the active drug to the experimental group and a matched placebo to the control group. All other conditions (e.g., clinic visits, dietary advice) are kept identical between groups [2].
- Blinding: Implement a double-blind procedure where neither the participants nor the researchers directly assessing the outcomes know which group a participant is in. This prevents bias in the reporting and measurement of the DV [2].
Phase 3: Data Collection and Analysis
- Measurement: Measure the DV in both groups at the end of the intervention period (and potentially at baseline and interim points) using the pre-specified tool [8].
- Statistical Analysis: Compare the average DV scores between the experimental and control groups using appropriate statistical tests (e.g., t-test, ANOVA) to determine if the difference is statistically significant [8] [4]. Advanced techniques like regression analysis may be used to control for any residual confounding [11].
Protocol for a Cohort Observational Study
A cohort study is a common type of observational design used to investigate the potential effects of an exposure in a naturalistic setting [2].
Phase 1: Study Design and Cohort Selection
- Research Question: Formulate a question about association, not causation. For example: "Is there an association between prolonged exposure to Substance A (IV) and the incidence of Disease B (DV)?"
- Cohort Assembly: Identify a large group of participants who are free of Disease B at the start of the study. Within this group, classify participants based on their pre-existing exposure to Substance A (the IV). This is a subject variable, as the researcher does not assign the exposure [8] [13].
- Matching: To control for key confounding variables (e.g., age, gender), researchers may "match" each exposed individual with one or more unexposed individuals who share similar characteristics [11].
Phase 2: Long-Term Follow-Up
Phase 3: Data Analysis and Interpretation
- Comparison: Calculate and compare the incidence rates of Disease B between the exposed and unexposed cohorts.
- Statistical Control: Use multivariate statistical models (e.g., regression analysis) to adjust for the influence of measured confounding variables (e.g., smoking status, diet) on the relationship between the IV and DV [11]. It is crucial to note that despite these adjustments, the study can only demonstrate correlation, as unmeasured or unknown confounders may still influence the results [2] [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting rigorous experimental research, particularly in biomedical and pharmacological contexts.
Table 2: Key Reagent Solutions for Experimental Research
| Reagent/Material | Function in Research |
|---|---|
| Active Pharmaceutical Ingredient (API) | The central independent variable in drug trials; the substance whose causal effect on a biological system or disease is being tested [2] [13]. |
| Placebo | An inert substance identical in appearance to the API. Serves as the control condition for the experimental group, allowing researchers to isolate the specific pharmacological effect of the API from psychological or placebo effects [2]. |
| Buffers and Solvents | Stable, biologically compatible solutions used to dissolve or dilute the API and placebo, ensuring accurate dosing and administration to experimental groups [2]. |
| Assay Kits | Pre-packaged reagents used to quantitatively measure the dependent variable(s), such as biomarker levels, enzyme activity, or cell viability, ensuring standardized and reliable outcome measurement [14]. |
| Cell Culture Media | A precisely formulated solution that provides essential nutrients to support the growth and maintenance of cell lines in in vitro studies, providing a controlled environment for testing the IV [2]. |
| Blocking Agents & Antibodies | Reagents used in immunoassays and histochemistry to reduce non-specific binding (blocking) and specifically detect target molecules (antibodies), enabling precise measurement of biological DVs [14]. |
From Theory to Practice: Implementing Robust Study Designs in Biomedical Research
Within the broader thesis on experimental tests versus natural observation research, observational studies represent a cornerstone of scientific inquiry in situations where randomized controlled trials (RCTs) are impractical, unethical, or impossible to conduct [15] [16]. While experimental studies actively intervene by assigning treatments to establish causality, observational studies take a more naturalistic approach by measuring exposures and outcomes as they occur in real-world settings without researcher intervention [17] [18]. This fundamental distinction positions observational research as the only practicable method for answering critical questions of aetiology, natural history of rare conditions, and instances where an RCT might be unethical [15] [19].
For researchers, scientists, and drug development professionals, understanding the precise applications, strengths, and limitations of different observational designs is crucial for both conducting and critically appraising scientific evidence. Three primary types of observational studies form the backbone of this methodological approach: cohort, case-control, and cross-sectional studies [20] [16] [21]. Each serves distinct research purposes and offers unique advantages for investigating relationships between exposures and outcomes in population-based research. These designs are collectively classified as level II or III evidence in the evidence-based medicine hierarchy, yet well-designed observational studies have been shown to provide results comparable to RCTs, challenging the notion that they are inherently second-rate [16].
Comparative Analysis of Observational Study Designs
The table below provides a comprehensive comparison of the three main observational study designs, highlighting their key characteristics, applications, and methodological considerations.
| Feature | Cohort Study | Case-Control Study | Cross-Sectional Study |
|---|---|---|---|
| Primary Research Objective | Study incidence, causes, and prognosis [15] | Identify predictors of outcome and study rare diseases [15] | Determine prevalence [15] |
| Temporal Direction | Prospective or retrospective [16] | Retrospective [15] | Single point in time [16] |
| Direction of Inquiry | Exposure → Outcome [16] | Outcome → Exposure [16] | Exposure & Outcome simultaneously [16] |
| Incidence Calculation | Can calculate incidence and relative risk [16] | Cannot calculate incidence [16] | Cannot calculate incidence [16] |
| Time Requirement | Long follow-up (prospective); shorter (retrospective) [22] | Relatively quick [22] | Quick and easy [15] |
| Cost Factor | Expensive (prospective); less costly (retrospective) [16] | Inexpensive [22] | Inexpensive [17] |
| Sample Size | Large sample size often needed [16] | Fewer subjects needed [17] | Variable, often large [17] |
| Ability to Establish Causality | Can suggest causality due to temporal sequence [15] | Cannot establish causality [15] | Cannot establish causality [15] |
| Key Advantage | Can examine multiple outcomes for a single exposure [16] | Efficient for rare diseases or outcomes with long latency [15] [16] | Provides a snapshot of population characteristics [22] |
| Primary Limitation | Susceptible to loss to follow-up (prospective) [16] | Vulnerable to recall and selection biases [16] [17] | Cannot distinguish cause and effect [15] |
Workflow and Temporal Relationships
The following diagram illustrates the fundamental temporal structures and participant flow characteristics that differentiate the three main observational study designs.
Detailed Examination of Study Designs
Cohort Studies
Cohort studies involve identifying a group (cohort) of individuals with specific characteristics in common and following them over time to gather data about exposure to factors and the development of outcomes of interest [23]. The term "cohort" originates from the Latin word cohors, referring to a Roman military unit, and in modern epidemiology defines "a group of people with defined characteristics who are followed up to determine incidence of, or mortality from, some specific disease, all causes of death, or some other outcome" [16].
Experimental Protocol for Prospective Cohort Studies:
- Population Definition: Identify and select a study population free of the outcome of interest at baseline [16]
- Exposure Assessment: Measure and document exposure status (exposed vs. unexposed) at the start of the investigation [16]
- Follow-up Period: Establish a predetermined follow-up duration with regular intervals for data collection [18]
- Outcome Measurement: Systematically measure and document outcome occurrence in both exposed and unexposed groups [16]
- Data Analysis: Compare incidence rates between groups to calculate relative risk and other measures of association [16]
Cohort studies can be conducted prospectively (forward-looking) or retrospectively (backward-looking) [16] [18]. Prospective designs, such as the landmark Framingham Heart Study, follow participants from the present into the future, allowing tailored data collection but requiring long follow-up periods [16]. Retrospective cohort studies use existing data to look back at exposure and outcome relationships, making them less costly and time-consuming but vulnerable to data quality issues [16]. A key methodological concern in prospective cohort studies is attrition bias, with a general rule suggesting loss to follow-up should not exceed 20% of the sample to maintain internal validity [16].
Case-Control Studies
Case-control studies work by identifying patients who have the outcome of interest (cases) and matching them with individuals who have similar characteristics but do not have the outcome (controls), then looking back to see if these groups differed regarding the exposure of interest [23]. This design is particularly valuable for studying rare diseases or outcomes with long latency periods where cohort studies would be inefficient [15] [16].
Experimental Protocol for Case-Control Studies:
- Case Definition: Establish clear diagnostic and eligibility criteria for case selection [16]
- Control Selection: Identify appropriate controls from the same source population as cases, matching for potential confounders like age and gender [20] [16]
- Exposure Assessment: Gather historical exposure data through interviews, medical records, or other sources for both groups [18]
- Blinding: Ensure researchers assessing exposure status are blinded to case/control status to minimize bias [16]
- Data Analysis: Calculate odds ratios to estimate the strength of association between exposure and outcome [16]
The case-control design is inherently retrospective, moving from outcome to exposure [16]. A major methodological challenge is the appropriate selection of controls, who should represent the source population that gave rise to the cases [16]. These studies are particularly vulnerable to recall bias, as participants with the outcome may remember exposures differently than controls, and confounding variables may unequally distribute between groups [17].
Cross-Sectional Studies
Cross-sectional studies examine the relationship between diseases and other variables as they exist in a defined population at one particular time, measuring both exposure and outcomes simultaneously [17]. These studies are essentially a "snapshot" of a population at a specific point in time [21].
Experimental Protocol for Cross-Sectional Studies:
- Population Sampling: Select a representative sample from the target population, often using random sampling methods [17]
- Single Time Point Assessment: Administer all measurements, interviews, or examinations at the same point in time [21]
- Data Collection: Gather information on both exposure/factor status and outcome/disease status concurrently [16]
- Prevalence Calculation: Determine disease prevalence and exposure prevalence within the sample [15]
- Association Analysis: Examine relationships between exposures and outcomes using statistical tests for association [17]
Because cross-sectional studies measure exposure and outcome simultaneously, they cannot establish temporality or distinguish whether the exposure preceded or resulted from the outcome [15] [16]. This fundamental limitation means they can establish association at most, not causality [17]. However, they are valuable for determining disease prevalence, assessing public health needs, and generating hypotheses for more rigorous studies [15] [20]. They are also susceptible to the "Neyman bias," a form of selection bias that can occur when the duration of illness affects the likelihood of being included in the study [17].
Research Reagent Solutions: Methodological Tools for Observational Research
The table below outlines essential methodological components and tools for conducting rigorous observational research, analogous to research reagents in laboratory science.
| Methodological Component | Function & Application | Study Design Relevance |
|---|---|---|
| Standardized Questionnaires | Ensure consistent, comparable data collection across all participants [22] | All observational designs, particularly cross-sectional studies [22] |
| Electronic Health Records (EHR) | Provide existing longitudinal data for retrospective analyses [16] | Retrospective cohort and case-control studies [16] |
| Matching Protocols | Minimize confounding by ensuring cases and controls are similar in key characteristics [20] [16] | Primarily case-control studies [16] |
| Follow-up Tracking Systems | Maintain participant contact and minimize loss to follow-up [16] | Prospective cohort studies [16] |
| Blinded Outcome Adjudication | Reduce measurement bias by concealing exposure status from outcome assessors [16] | Primarily cohort studies [16] |
| Statistical Analysis Plans | Pre-specified protocols for calculating measures of association and addressing confounding [16] [17] | All analytical observational designs [17] |
Decision Framework for Study Design Selection
The following diagram illustrates a systematic approach to selecting the most appropriate observational study design based on specific research questions and practical considerations.
Cohort, case-control, and cross-sectional studies collectively form an essential methodological toolkit for investigating research questions where randomized controlled trials are not feasible, ethical, or practical [15] [19]. Each design offers distinct advantages: cohort studies for establishing incidence and temporal relationships, case-control studies for efficient investigation of rare conditions, and cross-sectional studies for determining prevalence and generating hypotheses [15] [16]. The choice between these designs depends fundamentally on the research question, frequency of the outcome, available resources and time, and the specific information needs regarding disease causation or progression [18].
For researchers and drug development professionals, understanding the precise applications, strengths, and limitations of each observational design is crucial for both conducting rigorous studies and critically evaluating published literature. While observational studies cannot establish causality with the same reliability as well-designed RCTs, they provide invaluable evidence for understanding disease patterns, risk factors, and natural history [16] [18]. When designed and implemented with careful attention to minimizing bias and confounding, observational studies make indispensable contributions to evidence-based medicine and public health decision-making.
Randomized Controlled Trials (RCTs) are universally regarded as the gold standard for clinical research, providing the foundation for evidence-based medicine. Their design is uniquely capable of establishing causal inference between an intervention and an outcome, primarily through the use of randomization to minimize confounding bias. This guide explores the implementation of traditional RCTs, their core variations, and how they compare to observational studies within the broader landscape of clinical evidence generation.
The Core Principles and Regulatory Backbone of RCTs
An RCT is a true experiment in which participants are randomly allocated to receive either a specific intervention (the experimental group) or a different intervention (the control or comparison group). The scientific design hinges on two key components [24]:
- Randomized: Researchers decide randomly which participants receive the new treatment and which receive a placebo or reference treatment. This eliminates selection bias, preventing the deliberate or unconscious skewing of results by ensuring that known and unknown prognostic factors are balanced across groups. [25] [26] [24]
- Controlled: The trial uses a control group for comparison. This group may receive a placebo, an established standard of care, or no treatment. The control group is essential for determining whether observed effects can be genuinely attributed to the experimental intervention, as it accounts for other factors that could influence the outcome. [24]
Regulatory bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) generally require evidence from RCTs to approve new drugs and high-risk medical devices [27] [24]. This is because RCTs' internal validity offers the best assessment of a treatment's efficacy—whether it works under ideal and controlled conditions [28].
Variations on the Gold Standard: Adaptive and Streamlined Trial Designs
While the classic two-arm, parallel-group RCT is foundational, several innovative variations have been developed to enhance efficiency, ethics, and applicability.
Table 1: Key Variations of Randomized Controlled Trials
| Variation Type | Primary Objective | Key Features | Example Use Case |
|---|---|---|---|
| Adaptive Trials [26] | To create more flexible and efficient trials. | Pre-planned interim analyses allow for modifications (e.g., dropping ineffective arms, adjusting sample size) without compromising validity. | Evaluating multiple potential therapies for a new disease. |
| Platform Trials [26] [27] | To study an entire disease domain with a sustainable infrastructure. | Multiple interventions are compared against a common control arm. Interventions can be added or dropped over time based on performance. | The RECOVERY trial for COVID-19 treatments. [27] |
| Large Simple Trials [27] | To answer pragmatic clinical questions with high generalizability. | Streamlined design, minimal data collection, and use of routinely collected healthcare data (e.g., electronic health records, registries) to enroll large, representative populations quickly and cost-effectively. | The TASTE trial assessing a medical device for heart attack patients. [27] |
| Single-Arm Trials with External Controls [29] [30] | To provide evidence when a concurrent control group is unethical or infeasible. | All participants receive the experimental therapy. Their outcomes are compared to an externally sourced control group, often built from historical data like natural history studies or patient registries. | Trials for rare diseases, such as the approval of Zolgensma for spinal muscular atrophy. [30] |
Methodological Protocols: From Traditional to Modern RCTs
Protocol 1: The Traditional Two-Arm RCT
This is the foundational design for establishing efficacy [31].
- Protocol Development: A prospective study protocol is created with strict inclusion/exclusion criteria, a well-defined intervention, and pre-specified primary and secondary endpoints. [28]
- Randomization & Blinding: Eligible participants are randomly assigned to either the experimental or control group. Allocation concealment and blinding (single, double, or triple) are used to prevent bias. [31]
- Intervention & Follow-up: The assigned intervention is administered per protocol, and participants are followed for a pre-determined period.
- Outcome Assessment: Endpoints are measured and compared between the two groups. The primary analysis is typically conducted on an intention-to-treat basis.
Protocol 2: Large Simple RCT Using Real-World Data
This pragmatic design assesses effectiveness—how a treatment performs in real-world clinical practice [27].
- Streamlined Setup: Eligibility criteria are broad and inclusive to reflect a typical patient population. The trial is often embedded within healthcare systems.
- Minimal Site Workload: A one-page electronic case report form (eCRF) is used at key points (e.g., randomization, discharge/death). This was successfully implemented in the RECOVERY trial. [27]
- Routine Data Linkage: Follow-up data for key outcomes (e.g., all-cause mortality) are automatically supplemented through linkages to national healthcare databases, claims data, or disease registries, ensuring complete follow-up with minimal extra effort. [27]
- Analysis: The analysis focuses on a few important clinical outcomes collected from the linked databases.
Experimental vs. Control Group Workflow
The Scientist's Toolkit: Essential Reagents and Materials for Clinical Trials
Table 2: Key Research Reagents and Materials for Clinical Trials
| Item / Solution | Function in the Clinical Trial |
|---|---|
| Investigational Product | The drug, biologic, or device being tested. Its purity, potency, and stability are critical and must be manufactured under Good Manufacturing Practice (GMP). |
| Placebo | An inert substance or dummy device that is indistinguishable from the active product. It serves as the control to isolate the psychological and incidental effects from the true pharmacological effect of the intervention. [24] |
| Randomization System | A computerized or web-based system (e.g., Interactive Web Response System - IWRS) that ensures the unbiased allocation of participants to study arms, maintaining allocation concealment. |
| Electronic Data Capture (EDC) | A software system for collecting clinical data electronically. It streamlines data management, improves quality, and is essential for large simple trials using case report forms. [27] |
| Standard of Care Treatment | An established, effective treatment used as an active comparator in the control arm. This allows for a direct comparison of the new intervention's benefit against the current best practice. [24] |
| Protocol | The master plan for the entire trial. It details the study's objectives, design, methodology, statistical considerations, and organization, ensuring consistency and scientific rigor across all trial sites. [28] |
RCTs vs. Observational Studies: An Objective Data-Driven Comparison
The choice between an RCT and an observational study is dictated by the research question, with each playing a distinct role in the evidence ecosystem. RCTs are optimal for establishing efficacy under controlled conditions, while well-designed observational studies are invaluable for assessing effectiveness in real-world settings, long-term safety, and when RCTs are unethical or impractical [32] [26] [28].
A 2021 systematic review of 30 systematic reviews across 7 therapeutic areas provided a direct quantitative comparison, analyzing 74 pairs of pooled relative effect estimates from RCTs and observational studies [32]. The key findings are summarized below:
RCT vs. Observational Study Comparison
This data shows that while the majority of comparisons show no significant difference, a substantial proportion exhibit extreme variation, underscoring the potential for bias in observational estimates and the complementary roles of both designs [32].
Observational studies are particularly crucial in rare disease drug development, where patient populations are small and traditional RCTs may be infeasible. Regulatory approvals for drugs like Skyclarys (omaveloxolone) for Friedreich's ataxia and Zolgensma for spinal muscular atrophy have leveraged natural history studies as external controls in single-arm trials [29] [30].
Within the broader thesis on experimental tests versus natural observation research, the fundamental choice of methodology is dictated by the research question itself. This decision determines the quality of the evidence, the strength of the conclusions, and the very applicability of the findings to real-world scenarios. Experimental studies are characterized by the deliberate manipulation of variables under controlled conditions to establish cause-and-effect relationships [1] [33]. In contrast, observational studies involve measuring variables as they naturally occur, without any intervention from the researcher [1] [2]. This guide provides an objective comparison of these two methodological pillars, equipping researchers and drug development professionals with the criteria necessary to select the optimal design for their investigative goals.
Core Definitions and Methodological Frameworks
What is an Experimental Study?
An experimental study is a research design in which an investigator actively manipulates one or more independent variables to observe their effect on a dependent variable, typically with the goal of establishing a cause-effect relationship [1] [4]. The hallmarks of this approach include a high degree of control over the environment, and the random assignment of participants to different groups, such as an experimental group that receives the intervention and a control group that does not [1] [5].
Detailed Experimental Protocol: The Randomized Controlled Trial (RCT)
The RCT is considered the gold standard for experimental research in fields like medicine and pharmacology [5] [2]. The workflow can be summarized as follows:
Diagram 1: Experimental RCT Workflow.
Key aspects of this protocol include:
- Blinding: In single- or double-blind designs, participants and/or researchers are unaware of group assignments to prevent bias [2] [33].
- Control: Strict protocols ensure the environment and procedures are consistent for all groups, isolating the effect of the independent variable [1] [33].
What is an Observational Study?
An observational study is a non-experimental research method where the investigator observes subjects and measures variables of interest without assigning treatments or interfering with the natural course of events [1] [4]. The researcher's role is to document, rather than influence, what is occurring. These studies are primarily used to identify patterns, correlations, and associations in real-world settings [2].
Detailed Observational Protocol: The Cohort Study
A common and powerful observational design is the cohort study, which follows a group of people over time [5] [2]. The workflow is fundamentally different from an experiment:
Diagram 2: Observational Cohort Study Workflow.
Key aspects of this protocol include:
- No Manipulation: The researcher does not assign exposures (e.g., smoking, a specific diet); they merely record the existing exposures of the participants [1] [34].
- Natural Setting: Data collection occurs in the subject's environment, such as a clinic, workplace, or home, which provides high ecological validity [35] [36].
Objective Comparison: Experimental vs. Observational Studies
The following tables provide a structured, quantitative and qualitative comparison of the two methodologies, highlighting their distinct characteristics, strengths, and weaknesses.
Table 1: Core Characteristics and Methodological Rigor
| Aspect | Experimental Study | Observational Study |
|---|---|---|
| Variable Manipulation | Active manipulation of independent variable(s) [1] [33] | No manipulation; observes variables as they occur [1] [33] |
| Control Over Environment | High control; often in lab settings [1] [33] | Little to no control; natural, real-world settings [1] [33] |
| Random Assignment | Yes, participants are randomly assigned to groups [1] [5] | No random assignment; groups are pre-existing [4] |
| Ability to Establish Causation | High; can establish cause-and-effect [1] [2] | Low; can only identify correlations/associations [1] [5] |
| Use of Control Group | Yes, to compare against experimental group [1] [4] | Sometimes (e.g., in case-control studies), but not through assignment [5] |
| Key Research Output | Evidence of causal effect from intervention [2] | Evidence of a relationship or pattern between variables [2] |
Table 2: Practical Considerations, Validity, and Application
| Aspect | Experimental Study | Observational Study |
|---|---|---|
| Ecological Validity | Potentially low due to artificial, controlled setting [1] | High, as data is captured in real-world environments [1] [35] |
| Susceptibility to Bias | Risk of demand characteristics/experimenter bias [1] | Risk of observer, selection, and confounding bias [1] [5] |
| Ethical Considerations | Can be constrained; manipulation may be unethical [1] [4] | More ethical when manipulation is unsafe or unethical [2] [4] |
| Time & Cost | Often more time-consuming and costly [1] [5] | Generally less costly and faster to implement [1] [33] |
| Replicability | High, due to controlled conditions [1] | Low to medium, as natural conditions are hard to recreate [1] |
| Ideal Use Case | Testing hypotheses, particularly cause and effect [1] | Exploring phenomena in real-world contexts [1] |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and solutions central to conducting rigorous experimental research, particularly in drug development.
Table 3: Key Reagents and Materials for Experimental Research
| Reagent/Material | Primary Function in Research |
|---|---|
| Placebo | An inactive substance identical in appearance to the active drug, used in the control group to blind participants and researchers, isolating the pharmacological effect from the placebo effect [2]. |
| Active Comparator/Standard of Care | An established, effective treatment used in the control group to benchmark the performance and efficacy of a new experimental intervention [2]. |
| Blinding/Masking Protocols | Procedures (single- or double-blind) that ensure participants and/or investigators are unaware of treatment assignments to minimize bias in outcome assessment [2] [33]. |
| Randomization Schedule | A computer-generated or statistical plan that ensures each participant has an equal chance of being assigned to any study group, minimizing selection bias and balancing confounding factors [1] [5]. |
| Validated Measurement Instruments | Tools and assays (e.g., ELISA kits, PCR assays, clinical rating scales) that have been confirmed to accurately and reliably measure the dependent variables of interest [1]. |
The choice between an experimental and observational design is not a matter of which is superior, but of which is most appropriate for the research question at hand [1] [4].
Choose an experimental study when your objective is to establish causation, test a specific hypothesis about the effect of an intervention, and when it is ethically and practically feasible to manipulate variables and control the environment [33] [4]. This is the preferred methodology for definitive efficacy testing of new drugs and therapies [2].
Choose an observational study when your objective is to understand patterns, prevalence, and associations in a naturalistic context, when it would be unethical to manipulate the independent variable (e.g., studying the effects of smoking), or when studying long-term outcomes or rare events that are not feasible to replicate in a lab [2] [4]. This methodology is ideal for generating hypotheses, studying real-world effectiveness, and analyzing risk factors.
By systematically applying this framework and understanding the core protocols, comparisons, and tools outlined in this guide, researchers can make informed, strategic decisions that enhance the validity, impact, and applicability of their scientific work.
In drug development and clinical research, the choice between experimental tests and natural observation is fundamental, shaping the evidence generated and the decisions that follow. Experimental studies, characterized by active researcher intervention and variable manipulation, establish cause-and-effect relationships, making them the gold standard for demonstrating therapeutic efficacy. In contrast, observational studies gather data on subjects in their natural settings without intervention, providing critical real-world evidence on disease progression and treatment effectiveness in routine clinical practice [2] [37]. This guide objectively compares these methodologies through real-world case studies, detailing their protocols, applications, and performance in generating reliable evidence for the scientific community.
The distinction between these approaches is profound. Experimental designs, particularly randomized controlled trials (RCTs), exert high control, using randomization and blinding to minimize bias and confidently establish causality between an intervention and an outcome [2] [1]. Observational designs, such as cohort studies and case-control studies, forego such manipulation, instead seeking to understand relationships and outcomes as they unfold naturally in heterogeneous patient populations [2]. Each method contributes uniquely to the medical evidence ecosystem, and their comparative strengths and limitations are best illustrated through direct application in drug development.
Methodological Framework: Core Concepts and Definitions
Experimental Studies
An experimental study is defined by the active manipulation of one or more independent variables (e.g., a drug treatment) by the investigator to observe the effect on a dependent variable (e.g., disease symptoms) [2] [1]. The core objective is to establish a cause-and-effect relationship.
- Key Characteristics: Manipulation of variables, controlled environment, use of randomization and blinding, and the presence of a control group for comparison [37] [1].
- Primary Goal: To test specific hypotheses about the efficacy and safety of medical interventions.
- Common Designs: Randomized Controlled Trials (RCTs), crossover trials, and pragmatic trials [2].
Observational Studies
An observational study involves researchers collecting data without interfering or manipulating any variables [2] [35]. The goal is to understand phenomena and identify associations as they exist in real-world settings.
- Key Characteristics: No intervention, data collection in natural environments, and subjects are not assigned to specific treatments by the researcher [37].
- Primary Goal: To describe patterns, identify risk factors, and generate hypotheses, particularly when experiments are impractical or unethical.
- Common Designs: Cohort studies (prospective or retrospective), case-control studies, and cross-sectional studies [2].
The following workflow visualizes the fundamental decision-making process and structure of these two methodological approaches in clinical research.
Experimental Study Case Study: The Randomized Controlled Vaccine Trial
Experimental Protocol and Design
Vaccine trials represent a quintessential application of the experimental model, designed to provide definitive evidence of efficacy and safety [37].
- Hypothesis: A pre-specified, testable hypothesis is formulated, e.g., "The investigational vaccine reduces the incidence of disease X compared to a placebo."
- Randomization: Participants meeting strict inclusion/exclusion criteria are randomly assigned to either the investigational vaccine group or the control group (which receives a placebo or standard-of-care vaccine) [2] [1]. This minimizes selection bias and ensures groups are comparable at baseline.
- Blinding: The study is typically double-blinded, meaning neither the participants nor the investigators know who is receiving the vaccine or the placebo. This prevents bias in outcome assessment and reporting [2].
- Control Group: The use of a placebo control group is critical to isolate the specific effect of the vaccine from other factors and to account for the placebo effect [2].
- Data Collection: Participants are followed for a predetermined period to monitor for disease incidence (the primary efficacy outcome) and the occurrence of any adverse events (safety outcomes).
Performance and Outcomes
The experimental vaccine trial design delivers high-quality evidence for regulatory decision-making.
- Causal Inference: The combination of randomization, blinding, and a control group allows researchers to conclude that observed differences in disease incidence are causally related to the vaccine [2] [1].
- Minimized Bias: Blinding procedures significantly reduce the risk of performance and detection bias.
- Regulatory Approval: This rigorous design generates the evidence required by agencies like the FDA and EMA for approving new drugs and vaccines [2].
Table 1: Quantitative Outcomes from a Hypothetical Vaccine RCT
| Study Arm | Sample Size | Disease Incidence | Relative Risk Reduction | Common Adverse Event Rate |
|---|---|---|---|---|
| Vaccine Group | 15,000 | 0.1% | 95% | 15% |
| Placebo Group | 15,000 | 2.0% | - | 14% |
The Scientist's Toolkit: Research Reagent Solutions for an RCT
Table 2: Essential Materials for a Clinical Trial
| Item/Solution | Function in the Experiment |
|---|---|
| Investigational Product | The vaccine or drug whose safety and efficacy are being tested. |
| Placebo | An inert substance identical in appearance to the investigational product, used to blind the study and control for the placebo effect. |
| Randomization System | A computerized system to ensure each participant has an equal chance of being assigned to any study group, minimizing allocation bias. |
| Case Report Form (eCRF) | A standardized tool (increasingly electronic) for collecting accurate and comprehensive data from each participant throughout the trial. |
| Laboratory Kits | Standardized kits for processing and analyzing biological samples (e.g., serology for antibody titers). |
Observational Study Case Study: Naturalistic Research on Smoking and Lung Cancer
Observational Protocol and Design
The definitive link between smoking and lung cancer was established through large-scale, long-term observational cohort studies, as it would be unethical to randomly assign people to smoke [2] [37] [35].
- Study Design: Prospective Cohort Study. A large group of individuals who did not have cancer were enrolled and their smoking behaviors were assessed.
- Participant Selection: A sample was selected, often based on exposure (smokers and non-smokers), but without any intervention from the researchers [2].
- Data Collection: Researchers followed the cohort over many years (often decades), collecting data on who developed lung cancer and who did not. This is a key feature of cohort studies: following groups over time [2].
- Comparison: The incidence rate of lung cancer in the group of smokers was compared to the incidence rate in the group of non-smokers.
Performance and Outcomes
This naturalistic observation approach provides powerful real-world evidence but has inherent limitations.
- Real-World Insights: The study captured data in a natural environment, making the findings highly applicable to the general population (high external validity) [2] [35].
- Ethical Advantage: It allowed for the study of a harmful exposure without ethically imposing it on subjects [2].
- Identification of Association: The study identified a strong association between smoking and lung cancer, which was consistent across multiple studies, suggesting causality.
- Challenges: The study was susceptible to confounding variables (e.g., diet, occupational exposure to carcinogens) that could also influence lung cancer risk. While statistical methods can adjust for known confounders, residual confounding remains a limitation [2].
Table 3: Quantitative Outcomes from a Hypothetical Observational Cohort Study
| Cohort | Sample Size | Person-Years of Follow-up | Lung Cancer Cases | Incidence Rate per 10,000 PY |
|---|---|---|---|---|
| Smokers | 20,000 | 380,000 | 1,140 | 30.0 |
| Non-Smokers | 30,000 | 570,000 | 171 | 3.0 |
Comparative Analysis: Performance Data and Application Context
The following table provides a structured, side-by-side comparison of the two methodologies, summarizing their performance across key metrics relevant to researchers and drug development professionals.
Table 4: Direct Comparison of Experimental vs. Observational Study Designs
| Criteria | Experimental Study (e.g., RCT) | Observational Study (e.g., Cohort) |
|---|---|---|
| Researcher Control | Active manipulation of variables [37] | No manipulation; observation only [37] |
| Causality Establishment | Directly measured; can prove cause-and-effect [37] [1] | Limited or inferred; can only show association [37] [1] |
| Use of Randomization | Commonly used to minimize bias [2] | Not used; participants self-select or are selected based on exposure [2] |
| Internal Validity | High (controlled environment minimizes bias) [1] | Lower (susceptible to confounding and bias) [2] |
| External Validity / Generalizability | Sometimes limited due to strict inclusion criteria [2] [1] | Generally higher, as data comes from real-world settings [2] [1] |
| Ethical Considerations | Can be high (withholding treatment, potential side effects) [2] | Generally lower, as it studies natural courses [2] [37] |
| Primary Application in Drug Development | Regulatory approval; establishing efficacy and safety [2] | Post-marketing surveillance; long-term outcomes; comparative effectiveness [2] [38] |
| Resource Requirements | Higher due to controlled setup, monitoring, and interventions [2] [37] | Generally lower cost, though long-term follow-up can be expensive [37] [1] |
| Flexibility | Fixed, rigid protocol with limited flexibility after initiation [2] | More flexible design that can evolve during the study [35] |
Integrated Applications: Functional Service Providers in Modern Clinical Research
The execution of both experimental and observational studies in today's complex environment often involves specialized partners. Functional Service Providers (FSPs) have emerged as strategic partners for pharmaceutical sponsors, offering specialized services in specific functional areas like clinical monitoring, data management, biostatistics, and pharmacovigilance [39].
This model allows sponsors to access top-tier expertise and scalable resources, enhancing the quality and efficiency of research, whether it is a tightly controlled RCT or a large observational real-world evidence study [39]. Leading FSPs like IQVIA, Parexel, and ICON provide the operational excellence and analytical rigor required to manage the intricacies of modern clinical trials and the vast datasets generated by observational research [39] [40]. The trend toward leveraging such specialized partners underscores the growing sophistication and collaborative nature of drug development, where methodological purity is supported by optimized operational execution.
The dichotomy between experimental tests and natural observation is not a contest for superiority but a recognition of complementary roles in building robust medical evidence. As demonstrated through the vaccine trial and smoking study case studies, randomized controlled trials provide the rigorous, controlled environment necessary for establishing causal efficacy, forming the bedrock of regulatory approval. Conversely, observational studies offer indispensable insights into the long-term, real-world effectiveness and safety of interventions across diverse populations, guiding clinical practice and health policy.
A sophisticated drug development strategy intentionally leverages both. It uses experimental methods to confirm a drug's biological effect and then employs naturalistic observation to understand its full impact in the complex ecosystem of routine patient care. Together, these methodologies form a complete evidence generation cycle, driving innovation and improving patient outcomes.
Navigating Research Pitfalls: Strategies to Mitigate Bias and Enhance Study Validity
Observational studies are a cornerstone of research in fields such as epidemiology, sociology, and comparative effectiveness research, where randomized controlled trials (RCTs) are not always feasible or ethical [5]. Unlike experimental studies, where researchers assign interventions, observational studies involve classifying individuals as exposed or non-exposed to certain risk factors and observing outcomes without any intervention [41] [42]. This fundamental difference, while allowing for the investigation of important questions, introduces significant methodological challenges that can compromise the validity of the findings.
The two most pervasive threats to the validity of observational studies are confounding and selection bias [43] [44]. Confounding can create illusory associations or mask real ones, while selection bias can render a study population non-representative, leading to erroneous conclusions [45] [46]. Understanding, identifying, and mitigating these biases is paramount for researchers who rely on observational data to guide future research or inform clinical and policy decisions. This guide explores these challenges within the broader context of comparing the robustness of experimental tests versus natural observation research, providing a detailed overview of strategies to enhance the reliability of observational study findings.
Understanding Confounding
Definition and Core Principles
Confounding derives from the Latin confundere, meaning "to mix" [41]. It is a situation in which a non-causal association between an exposure and an outcome is observed because of a third variable, known as a confounder. For a variable to be a confounder, it must meet three specific criteria, as shown in the causal diagram below.
Causal Pathways in Confounding
A confounder is a risk factor for the outcome that is also associated with the exposure but does not reside in the causal pathway between the exposure and the outcome [41] [47]. For example, in an investigation of the association between coffee consumption and heart disease, smoking status could be a confounder. Smoking is a known cause of heart disease and is also associated with coffee-drinking habits, yet it is not an intermediate step between drinking coffee and developing heart disease [43]. If not accounted for, this confounding could make it appear that coffee causes heart disease.
Common Types of Confounding in Research
Several specific types of confounding frequently arise in observational studies of medical treatments:
- Confounding by Indication: This is one of the most common forms of bias in pharmacoepidemiology. It occurs when the clinical indication for prescribing a treatment is itself a risk factor for the outcome [47]. For instance, if a study finds that aldosterone antagonist use is associated with higher mortality in heart failure patients, it may be because clinicians preferentially prescribe this drug to sicker patients with more severe heart failure. The underlying disease severity confounds the association between the drug and mortality.
- Confounding by Frailty: This occurs because frail patients, who have a poor short-term prognosis, are less likely to receive preventive therapies than healthier individuals [47]. This can make a preventive treatment appear more beneficial than it truly is. For example, the observed large mortality reduction from influenza vaccination in older adults in some studies may be partly due to this bias, as the frailest individuals are less likely to be vaccinated.
- Healthy Adherer Effect: This arises when patients who adhere to a prescribed medication are also more likely to engage in other healthy behaviors (e.g., exercise, healthy diet) that improve their outcomes [47]. Studies comparing adherers to non-adherers may overestimate the drug's benefit because it is confounded by overall healthy behavior.
- Time-Varying Confounding: This occurs when the exposure and confounders change over time. A classic example is the study of erythropoietin-stimulating agent (ESA) dose and mortality in hemodialysis patients. Serum hemoglobin is a time-varying confounder: it influences ESA dosing, is affected by prior ESA dose, and is independently associated with mortality [47].
Methodological Strategies to Control for Confounding
Researchers can address confounding during both the design and analysis phases of a study. The following table summarizes common strategies.
Table 1: Strategies for Addressing Confounding in Observational Studies
| Phase | Method | Overview | Advantages | Disadvantages |
|---|---|---|---|---|
| Design | Restriction | Setting specific criteria for study inclusion. | Easy to implement. | Reduces sample size and generalizability; only controls for the restricted factor. |
| Matching | Creating matched sets of exposed and unexposed patients with similar confounder values. | Intuitive; can improve comparability. | Difficult to match on many factors; unmatched subjects are excluded. | |
| Active Comparator | Comparing the treatment of interest to another active treatment for the same condition. | Mitigates confounding by indication; clinically relevant. | Not possible if no alternative treatment exists. | |
| Analysis | Multivariable Adjustment | Including potential confounders as covariates in a regression model. | Easy to implement with standard software. | Only controls for measured confounders; limited by the number of outcome events. |
| Propensity Score Methods | Using a summary score (the propensity to be exposed) to match or weight groups. | Useful with many confounders; allows balance checking. | Only controls for measured confounders; may exclude subjects. | |
| G Methods | Advanced analytic techniques (e.g., g-computation) for time-varying confounding. | Appropriately handles complex time-varying confounding. | Complex; requires advanced statistical expertise. |
The choice of method depends on the research question, data structure, and available sample size. A key limitation shared by all analytic methods is that they can only adjust for measured confounders; unmeasured confounders remain a persistent threat to validity [47].
Understanding Selection Bias
Definition and Core Principles
Selection bias occurs when the process of selecting subjects into a study, or the likelihood of them remaining in the study, leads to a systematic difference between the study population and the target population [46] [48]. This bias arises because the relationship between exposure and outcome observed in the selected sample is not representative of the relationship in the population of interest. The mechanism of selection bias often involves a factor that influences both participation and the outcome, as illustrated below.
Mechanism of Selection Bias
When this happens, the study sample is no longer a random sample from the target population, and the estimated effect of the exposure on the outcome is distorted [46]. For example, if a study on cognitive decline in the elderly only includes healthy volunteers, the results will not be generalizable to all elderly people, as the sickest individuals may have died before they could be enrolled or may be unable to participate [48].
Common Types of Selection Bias
Selection bias can manifest in several forms throughout the research process:
- Sampling/Ascertainment Bias: Occurs when some members of the intended population are systematically less likely to be included than others [46]. For instance, a door-to-door survey of Parkinson's disease prevalence might miss individuals who are institutionalized or too ill to participate, leading to an underestimate of the true prevalence [48].
- Self-Selection/Volunteer Bias: Arises when individuals decide for themselves whether to participate [46]. Volunteers for health studies are often more health-conscious and have healthier behaviors than non-participants, leading to a "healthy participant effect" [48].
- Attrition Bias: Occurs when participants who drop out of a longitudinal study are systematically different from those who complete it [46]. For example, in a clinical trial, participants who experience side effects or find the treatment ineffective may be more likely to withdraw, skewing the final results.
- Nonresponse Bias: Similar to self-selection, this occurs when people who do not respond to a survey differ significantly from those who do [46].
- Immortal Time Bias: A specific and common bias in retrospective cohort studies where a period of follow-up time during which the outcome could not have occurred is misclassified [44]. A 2021 meta-research study found that 25% of observational studies using routinely collected data were at high risk of this bias [44].
Comparative Analysis: Observational vs. Experimental Studies
The fundamental difference between observational and experimental studies lies in the researcher's control over the intervention. This difference is the root cause of the heightened susceptibility of observational studies to confounding and selection bias.
Key Methodological Differences
In experimental studies, such as Randomized Controlled Trials (RCTs), the investigator actively assigns participants to intervention or control groups using randomization [5] [42]. This process is designed to ensure that both known and unknown confounding factors are, on average, evenly distributed between the groups. Furthermore, rigorous inclusion/exclusion criteria and intention-to-treat analysis help minimize selection and attrition biases [48].
In contrast, observational studies examine associations without assigning interventions. The researcher is a passive observer, classifying individuals based on their exposures or characteristics [42]. This lack of randomization is the primary reason why confounding is a more critical issue in observational studies [41]. Similarly, the inability to control participant recruitment and retention often leads to greater selection bias.
Strength of Evidence and Limitations
The RCT is widely considered the "gold standard" for establishing causal relationships because its design minimizes bias and allows for a fair comparison between groups [5] [42]. The following table provides a direct comparison of the two approaches.
Table 2: Comparison of Observational and Experimental Study Designs
| Aspect | Observational Studies | Experimental Studies (RCTs) |
|---|---|---|
| Intervention Assignment | Not assigned by researcher; natural or self-selected. | Randomly assigned by researcher. |
| Control for Confounding | Relies on statistical adjustment; only for measured variables. | Achieved via randomization; balances both known and unknown factors. |
| Risk of Selection Bias | High, due to non-random recruitment and retention. | Lower, due to randomized recruitment and intention-to-treat analysis. |
| Causal Inference | Can show association, but causation is difficult to prove. | Strong ability to establish causation. |
| External Validity | Often higher; results may be more generalizable to real-world populations. | Can be lower due to strict eligibility and artificial settings. |
| Ethical & Practicality | Only option for many questions (e.g., harmful exposures, rare diseases). | Not ethical or feasible for all research questions. |
| Example | Comparing outcomes of smokers vs. non-smokers. | Randomizing participants to a new drug or placebo. |
However, observational studies are indispensable. They are the only ethical choice for investigating harmful exposures (e.g., the link between smoking and lung cancer) and are crucial for studying rare diseases, long-term outcomes, and the effectiveness of treatments in real-world clinical practice [43] [5] [42]. While experimental studies have higher internal validity (confidence that the result is correct for the study population), observational studies can have greater external validity (generalizability to the wider population) [42].
The Researcher's Toolkit: Protocols and Reagents for Robust Studies
To enhance the validity of observational research, methodologies themselves can be considered part of the essential "toolkit." The following table outlines key conceptual "reagents" and their functions in combating bias.
Table 3: Essential Methodological Toolkit for Mitigating Bias in Observational Studies
| Tool/Reagent | Primary Function | Application Context |
|---|---|---|
| Target Trial Framework | A protocol for designing an observational study to emulate a hypothetical RCT. | Study planning; ensures alignment of eligibility, treatment assignment, and follow-up start to minimize selection and immortal time bias [44]. |
| Propensity Score | A statistical score representing the probability of being exposed given a set of baseline characteristics. | Analysis phase; used for matching or weighting to create a balanced comparison group that mimics randomization [47]. |
| Multivariable Regression Model | A statistical model that estimates the relationship between exposure and outcome while adjusting for multiple confounders simultaneously. | Analysis phase; controls for measured confounders to isolate the effect of the primary exposure [42] [47]. |
| Sensitivity Analysis | A set of analyses to assess how robust the study results are to potential unmeasured confounding or other biases. | Post-analysis; quantifies how strong an unmeasured confounder would need to be to explain away the observed association [48]. |
| RECORD Reporting Guideline | A checklist for reporting observational studies using routinely collected data. | Manuscript preparation; enhances research transparency and reproducibility [44]. |
Application Protocol: The Target Trial Framework
A powerful protocol for strengthening observational studies is the "target trial" framework developed by Hernán et al. [44]. This involves:
- Explicitly Specifying a Hypothetical RCT: Researchers begin by meticulously defining the protocol of a target trial they would ideally conduct—including eligibility criteria, treatment strategies, assignment procedures, follow-up start, outcomes, and causal contrast.
- Emulating the Trial with Observational Data: The observational study is then designed to mirror this hypothetical trial as closely as possible. This includes synchronizing the time of eligibility, treatment assignment, and the start of follow-up to mimic randomization.
- Addressing Discrepancies: The framework forces researchers to identify and, if possible, correct for inherent discrepancies between the observational data and the ideal trial (e.g., using the methods in Table 1).
This approach reduces the risk of biases like immortal time and selection bias by ensuring the study design, rather than just the analysis, is sound [44]. A 2021 review found that failure to apply this framework led to a high risk of bias in 25% of published observational studies using routinely collected data [44].
Confounding and selection bias are fundamental challenges that distinguish observational studies from experimental ones. Confounding mixes the effect of an exposure with other factors, while selection bias distorts the study population. While statistical methods like multivariable adjustment and propensity scores offer ways to mitigate these biases, they are imperfect, primarily because they cannot fully account for unmeasured factors.
The recognition of these limitations is not a dismissal of observational research but a call for rigorous methodology. The strategic use of the researcher's toolkit—including the target trial framework for design, robust statistical methods for analysis, and sensitivity analyses for interpretation—is critical for producing reliable evidence. For the scientific community, a thorough understanding of these challenges is essential for the critical appraisal of literature and for making informed decisions in drug development and clinical practice when the gold standard of randomization is not an option.
In the pursuit of scientific evidence, researchers must navigate a complex landscape of methodological trade-offs. The spectrum of research designs ranges from highly controlled experimental tests to naturalistic observational studies, each with distinct advantages and limitations. True experimental designs, characterized by random assignment and controlled conditions, establish high internal validity but often struggle with artificial settings that limit real-world applicability [49]. Conversely, natural observations excel at capturing authentic behaviors within their natural context but provide less rigorous control for establishing causal relationships. This article examines the core limitations of experimental designs, with particular focus on how ethical constraints and generalizability concerns shape their utility in scientific research and drug development.
Core Limitations of Experimental Designs
Controlled Environment Constraints
Experimental research typically occurs in controlled environments where variables are carefully monitored and manipulated. While this control allows researchers to isolate cause-and-effect relationships, it creates an artificial setting that fails to capture the complexity of real-world conditions [49]. This limitation is particularly problematic in health services research, where interventions that prove effective under ideal laboratory conditions may fail when implemented in routine clinical practice with its resource constraints and diverse patient populations [50]. The very controls that strengthen internal validity may simultaneously weaken the practical relevance of findings.
Ethical Constraints in Experimental Research
Ethical considerations present significant limitations across all research domains, particularly in drug development and medical research. Experimental designs often face ethical constraints in terms of assigning participants to different groups or manipulating variables [51]. Researchers may be limited in their ability to implement specific interventions or treatments due to ethical concerns, which impacts both the validity and generalizability of findings [51]. In medical contexts, ethical limitations include:
- Inability to withhold proven treatments from control groups
- Restrictions on manipulating potentially harmful variables
- Constraints on randomizing potentially beneficial interventions
- Limited access to vulnerable populations for experimental studies
These ethical boundaries often make true experimental designs infeasible, requiring researchers to seek alternative methodological approaches.
Generalizability and External Validity Concerns
Generalizability issues represent a fundamental limitation of experimental designs [49]. Controlled environments can lead to oversimplified scenarios that do not reflect real-world complexities, restricting what researchers call ecological validity [49]. Several factors contribute to this limitation:
- Homogeneous samples that do not represent broader populations
- Artificial settings that influence participant behavior differently than natural environments
- Standardized procedures that lack the variability of real-world conditions
- Limited contextual factors that would normally influence outcomes in natural settings
The challenge of generalizability is particularly acute in pharmaceutical research, where drugs tested on highly selected patient populations under ideal conditions may demonstrate different efficacy and safety profiles when prescribed to diverse patient groups in community practice settings.
Quasi-Experimental Designs: Balancing Rigor and Feasibility
Quasi-experimental designs occupy the methodological middle ground between true experiments and natural observations. These designs "lie between the rigor of a true experimental method (true experimental design includes random assignment to at least one control and one experimental/interventional group) and the flexibility of observational studies" [7]. Unlike true experiments, quasi-experimental designs do not involve random assignment, but they do involve some form of intervention or planned manipulation [7]. Common quasi-experimental designs include:
- Posttest-only design with a control group: Two groups (experimental and control) are measured after an intervention, without pretest measurements [7]
- One-group pretest-posttest design: Participants are measured before and after an intervention, without a separate control group [7]
- Pretest and posttest design with a control group: Both treatment and control groups complete measurements before and after the intervention [7]
These designs are particularly valuable when random assignment is impossible due to practical constraints.
Disadvantages of Quasi-Experimental Approaches
While quasi-experimental designs offer practical advantages, they come with significant methodological limitations that researchers must acknowledge.
Table 1: Key Disadvantages of Quasi-Experimental Designs
| Disadvantage | Description | Impact on Research |
|---|---|---|
| Lack of Randomization | Participants are not randomly assigned to treatment and control groups [51]. | Introduces potential for selection biases, as groups may differ in ways that affect outcomes [51]. |
| Internal Validity Concerns | Susceptible to threats like history, maturation, selection bias, and regression to the mean [51]. | Challenging to attribute observed effects solely to the treatment being studied [51]. |
| Limited Control over Extraneous Variables | Reduced ability to manage outside influences that can affect outcomes [51]. | Difficult to isolate effects of the independent variable; increased risk of confounding factors [51]. |
| Limited Causal Inferences | Establishing causal relationships is difficult due to design limitations [51]. | While valuable insights can be gained, these designs often fall short of providing strong evidence for causal claims [51]. |
These limitations necessitate careful design considerations and cautious interpretation of results when employing quasi-experimental approaches.
Quantitative Analysis in Experimental Research
Analytical Foundations
Quantitative data analysis serves as the foundation for evaluating experimental outcomes, employing mathematical, statistical, and computational techniques to examine numerical data [52]. In experimental research, quantitative analysis helps researchers uncover patterns, test hypotheses, and support decision-making through measurable information such as counts, percentages, and averages [52]. The two primary branches of statistical analysis include:
Descriptive Statistics: These summarize and describe the characteristics of a dataset using measures such as mean, median, mode, standard deviation, and range [52] [53]. They help researchers understand the central tendency, spread, and shape of their data [53].
Inferential Statistics: These use sample data to make generalizations, predictions, or decisions about a larger population [52] [53]. Key techniques include hypothesis testing, t-tests, ANOVA, regression analysis, and correlation analysis [52].
Table 2: Common Quantitative Analysis Methods in Experimental Research
| Method | Purpose | Application in Experimental Research |
|---|---|---|
| Cross-Tabulation | Analyzes relationships between categorical variables [52]. | Useful in analyzing survey data, market research, and consumer behavior; helps determine which interventions resonate with specific demographics. |
| T-Tests and ANOVA | Determine whether significant differences exist between groups or datasets [52]. | Essential for comparing experimental and control groups; assesses intervention effectiveness across multiple conditions. |
| Regression Analysis | Examines relationships between dependent and independent variables to predict outcomes [52]. | Models how changes in intervention components affect outcomes; identifies key factors driving experimental results. |
| Gap Analysis | Compares actual performance to potential or goals [52]. | Identifies discrepancies between expected and observed outcomes; highlights areas for intervention improvement. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Experimental Research
| Tool/Reagent | Function | Application Context |
|---|---|---|
| SPSS | Advanced statistical modeling and analysis [52]. | Powerful software for complex statistical analyses in experimental research, including ANOVA, regression, and factor analysis. |
| R Programming | Open-source statistical computing and data visualization [52]. | Flexible environment for implementing custom statistical analyses and creating publication-quality visualizations. |
| Python (Pandas, NumPy, SciPy) | Handling large datasets and automating quantitative analysis [52]. | Programming libraries ideal for managing complex experimental data, performing statistical tests, and building analysis pipelines. |
| ChartExpo | Creating advanced visualizations without coding [52]. | User-friendly tool for generating insightful charts and graphs directly within Excel, Google Sheets, and Power BI. |
| Microsoft Excel | Basic statistical analysis, pivot tables, and charts [52]. | Accessible platform for preliminary data analysis, descriptive statistics, and straightforward experimental comparisons. |
Optimisation Approaches in Health Intervention Research
The Optimisation Framework
Optimisation represents an emerging approach to addressing limitations in traditional experimental designs, particularly in health intervention research. Defined as "a deliberate, iterative and data-driven process to improve a health intervention and/or its implementation to meet stakeholder-defined public health impacts within resource constraints" [50], optimisation acknowledges the complex trade-offs inherent in intervention research. This approach recognizes that constraints may include time, cost, or intervention complexity [50], and seeks to develop interventions that are not only effective but also feasible and sustainable in real-world settings.
Optimisation typically employs cyclic processes that involve multiple evaluations of interventions and implementation strategies, modifications, and re-testing under constraint considerations until pre-specified outcomes are achieved [50]. This represents a departure from traditional linear research models and offers promise for developing interventions that maintain scientific rigor while enhancing practical applicability.
Methodological Innovations in Optimisation Trials
Recent systematic reviews of optimisation trials reveal interesting patterns in methodological approaches. Factorial designs are the most common design used to evaluate optimisation of an intervention (41%), whereas pre-post designs are the most common for implementation strategies (46%) [50]. This distribution reflects the different constraints and considerations applicable to intervention components versus implementation strategies.
However, current optimisation practice reveals significant methodological gaps. Only 11% of trials clearly defined optimisation success, and just 24% used a framework to guide the optimisation process [50]. This suggests substantial room for methodological refinement in optimisation research. The review recommends "the use of optimisation frameworks and a clear definition of optimisation success, as well as consideration of alternate methods such as adaptive designs, Bayesian statistics, and consolidating samples across research groups to overcome the impediments to evaluating optimisation success" [50].
Visualizing Research Design Trade-Offs
The following diagram illustrates the key relationships and trade-offs between different research design characteristics, using the specified color palette to enhance clarity while maintaining accessibility.
Research Design Trade-offs Diagram
Experimental designs face significant limitations in ethical constraints and generalizability that researchers must thoughtfully address. While true experimental designs provide methodological rigor through controlled conditions and random assignment, these very features can limit their applicability to real-world contexts and raise ethical concerns in many research scenarios. Quasi-experimental designs offer a practical alternative when random assignment is impossible but introduce their own limitations in establishing causal inference. The emerging framework of intervention optimisation represents a promising approach to addressing these challenges through deliberate, iterative processes that explicitly acknowledge resource constraints and implementation realities. For researchers and drug development professionals, selecting an appropriate research design requires careful consideration of these trade-offs, with particular attention to how methodological decisions impact both scientific validity and practical relevance in their specific research context.
Within the broader framework of scientific inquiry, a fundamental distinction exists between natural observation research and controlled experimental tests. Observational studies involve monitoring subjects and collecting data without interference, allowing researchers to identify correlations and generate hypotheses from real-world data [2] [4]. In contrast, experimental tests actively manipulate one or more variables under controlled conditions to establish cause-and-effect relationships [2] [4]. For these experiments to yield valid and reliable evidence, they rely on foundational optimization techniques to mitigate bias and confounding. Blinding, randomization, and statistical adjustment represent the core methodological pillars that uphold the integrity of experimental research, particularly in fields like clinical medicine and drug development [54] [55]. This guide provides a comparative analysis of these three critical techniques, detailing their protocols, applications, and contributions to scientific rigor.
Blinding in Experimental Research
Core Concept and Rationale
Blinding (or masking) is the process of concealing information about the assigned interventions from one or more parties involved in a research study from the time of group assignment until the experiment is complete [56]. This technique is crucial because knowledge of treatment assignment can lead to conscious or unconscious biases that quantitatively affect study outcomes [56] [57]. For instance, non-blinded participants may report exaggerated treatment effects, while unblinded outcome assessors may generate hazard ratios exaggerated by an average of 27% [56]. Blinding thus protects the internal validity of an experiment by ensuring that differences in outcomes can be attributed to the intervention itself rather than to expectations or differential treatment.
Detailed Experimental Protocol
Implementing blinding requires strategic planning tailored to the type of intervention:
Pharmaceutical Trials: The most common method uses centralized preparation of identical capsules, tablets, or syringes containing either active treatment or placebo [56] [58]. For treatments with distinctive tastes or smells, flavoring agents can mask these characteristics. The double-dummy technique is employed when comparing treatments with different administration routes (e.g., oral tablet vs. intramuscular injection); participants receive both an oral placebo (if assigned to injection) and an injection placebo (if assigned to oral medication), thus maintaining the blind [56].
Surgical and Device Trials: Blinding these interventions presents unique challenges but remains feasible through innovative methods. Using sham procedures (placebo surgery) where identical incisions are made without performing the actual intervention controls for placebo effects [56] [57]. Other techniques include covering incisions with standardized dressings to conceal scar appearance and digitally altering radiographs to hide implant types from outcome assessors [57].
Outcome Assessment Blinding: Independent adjudicators unaware of treatment allocation should assess endpoints, particularly when measurements involve subjectivity (e.g., radiographic progression, clinical symptom scores) [56] [57]. This is often achieved through centralized assessment of complementary investigations and clinical examinations.
Comparative Analysis of Blinding Approaches
Table 1: Comparison of Blinding Techniques Across Trial Types
| Technique | Primary Use Case | Key Methodology | Advantages | Limitations |
|---|---|---|---|---|
| Placebo-Controlled | Pharmaceutical trials | Identical physical characteristics (appearance, taste, smell) between active drug and placebo | High blinding integrity; Well-understood methodology | Matching physical characteristics can be complex and costly |
| Double-Dummy | Trials with different administration routes | Each participant receives both active and placebo versions of compared interventions | Allows comparison of dissimilar treatments; Maintains blinding | Increased participant burden; Higher medication management complexity |
| Sham Procedure | Surgical & device trials | Simulated procedure without therapeutic effect | Controls for placebo effect of intervention; Minimizes performance bias | Ethical concerns; Additional risk to participants without benefit |
| Assessor Blinding | All trial types with subjective endpoints | Independent evaluators unaware of treatment allocation | Reduces detection bias; Feasible even when participant blinding isn't possible | Does not prevent performance bias; Requires additional resources |
Randomization in Experimental Research
Core Concept and Rationale
Randomization is the random allocation of participants in a trial to different interventions, which is fundamental for producing high-quality evidence of treatment differences [54]. This technique serves two critical purposes: it eliminates subjective influence in assignment, and it ensures that known and unknown confounding factors are similarly distributed across intervention groups [54] [59] [55]. Through the introduction of a deliberate element of chance, randomization provides a sound statistical basis for evaluating treatment effects and permits the use of probability theory to express the likelihood that observed differences occurred by chance [59] [55].
Detailed Experimental Protocol
Various randomization procedures with different statistical properties are available:
Simple (Unrestricted) Randomization: This approach is equivalent to tossing a coin for each participant, typically implemented using computer-generated random numbers or random number tables [54] [59]. While conceptually straightforward and easy to implement, simple randomization can lead to substantial imbalance in group sizes, particularly in small trials [54] [59].
Restricted Randomization (Blocking): To maintain balance in group sizes throughout the recruitment period, restricted randomization uses blocks of predetermined size [54] [55]. For example, in a block of size 4 for two groups (A and B), there will be exactly two A's and two B's in random order. This ensures perfect balance after every completed block, though fixed block sizes can potentially allow prediction of future assignments if the block size becomes known [54].
Stratified Randomization: For known important prognostic factors (e.g., disease severity, age groups, study center), stratified randomization performs separate randomizations within each stratum [54] [55]. This ensures balance for these specific factors across treatment groups, which is particularly valuable in smaller trials where simple randomization might lead to chance imbalances [54].
Centralized randomization systems are now commonly used in large trials, where investigators telephone or electronically notify a central office after determining a participant's eligibility, and receive the random assignment [54]. This approach completely separates the enrollment process from the allocation process, minimizing potential for bias.
Comparative Analysis of Randomization Methods
Table 2: Comparison of Randomization Techniques in Clinical Trials
| Method | Procedure | Balance/Randomness Tradeoff | Ideal Application Context |
|---|---|---|---|
| Simple Randomization | Each assignment is independent, with equal probability for all groups | High randomness, but potential for sizeable imbalance in small samples | Large trials (hundreds of participants) where chance imbalance is minimal |
| Permuted Block Randomization | Assignment made in blocks with fixed ratio within each block | Guarantees periodic balance but reduces randomness, especially with small blocks | Small trials and stratified trials where balance over time is crucial |
| Stratified Randomization | Separate randomization schedule for each prognostic stratum | Balances specific known factors while maintaining randomness for others | When 2-3 important prognostic factors are known; Multicenter trials |
| Adaptive Randomization | Allocation probabilities adjust based on previous assignments or accumulating data | Dynamic balance across multiple factors; Complex implementation | Trials with many important prognostic factors; Small population trials |
Diagram 1: Randomization implementation workflow showing key decision points in selecting and applying different randomization methods.
Statistical Adjustment Methods
Core Concept and Rationale
Statistical adjustment methods are analytical techniques used to account for confounding factors and imbalances that may persist despite randomization, particularly in smaller studies [54] [55]. These methods help isolate the true effect of the intervention by controlling for the influence of other variables that might affect the outcome. While randomization aims to balance both known and unknown confounders, statistical adjustment provides a means to address residual imbalance in known prognostic factors during the analysis phase [54].
Detailed Analytical Protocol
Common statistical adjustment approaches include:
Regression Analysis: This encompasses a family of methods that model the relationship between the outcome variable and the intervention while adjusting for other covariates. Multiple linear regression is used for continuous outcomes, while logistic regression is employed for binary outcomes [4]. These methods estimate the intervention effect while holding the adjusted covariates constant statistically.
Analysis of Covariance (ANCOVA): This technique adjusts for baseline differences in continuous covariates when comparing treatment groups on a continuous outcome measure. ANCOVA increases statistical power by reducing within-group variance and providing unbiased estimates of treatment effects when baseline characteristics are imbalanced by chance [55].
Stratified Analysis: Rather than adjusting mathematically in a model, this approach evaluates treatment effects within homogeneous subgroups defined by important prognostic factors. The Mantel-Haenszel method is a common technique for combining these stratum-specific estimates into an overall adjusted treatment effect [55].
Randomization-Based Inference: As an alternative to model-based approaches, randomization tests use the actual randomization scheme to generate a reference distribution for the test statistic under the null hypothesis, providing a robust method that does not rely on distributional assumptions [55].
Comparative Analysis of Adjustment Methods
Table 3: Comparison of Statistical Adjustment Techniques
| Method | Underlying Principle | Data Requirements | Strengths | Weaknesses |
|---|---|---|---|---|
| Multiple Regression | Models outcome as a function of treatment and covariates | Continuous or categorical outcomes and predictors | Adjusts for multiple confounders simultaneously; Provides effect estimates | Assumes specific model structure; Sensitive to multicollinearity |
| ANCOVA | Adjusts group means based on relationship with continuous covariate | Continuous outcome and continuous baseline covariate | Increases power by reducing error variance; Handles baseline imbalance | Assumes linear relationship and homogeneity of slopes |
| Stratified Analysis | Estimates treatment effect within homogeneous subgroups | Sufficient sample size within strata | Nonparametric; Intuitive interpretation | Limited number of adjustible factors; Can suffer from sparse data |
| Propensity Score Methods | Balances covariates based on probability of treatment assignment | Multiple covariates for score estimation | Can handle numerous confounders; Mimics randomization | Complex implementation; Relies on correct model specification |
Integrated Application in Research Design
Synergistic Implementation
The true power of these optimization techniques emerges when they are strategically combined in research design. Randomization forms the foundation by initially balancing known and unknown confounders [54] [55]. Blinding then preserves this balance during trial execution by preventing differential treatment and assessment [56] [57]. Statistical adjustment serves as a final safeguard during analysis, addressing any residual imbalances and refining effect estimates [54] [55]. This multi-layered approach creates a robust defense against various forms of bias throughout the research process.
Diagram 2: Integrated bias control framework showing how randomization, blinding, and statistical adjustment address different bias risks across research phases.
Contextual Application Guidelines
The optimal application of these techniques varies by research context:
Pharmaceutical Clinical Trials: Represent the gold standard for implementation, typically employing complete blinding (double-blind design) with stratified randomization and covariate-adjusted analysis [56] [58] [55]. The high stakes of drug approval and substantial resources available enable comprehensive implementation of all three optimization methods.
Surgical and Device Trials: Often face practical limitations for full blinding of surgeons and participants [56] [57]. In these contexts, expertise-based trial designs (where surgeons only perform one procedure) combined with blinded outcome assessment and statistical adjustment provide viable alternatives [57].
Small Sample Size Studies: Randomization may not perfectly balance baseline characteristics in small studies, making stratified randomization and subsequent statistical adjustment particularly important [54] [55]. Blinding remains critical as its protective effect against bias is independent of sample size.
Observational Studies: While randomization is not possible in observational research, techniques like propensity score matching attempt to statistically recreate randomization, and blinding of outcome assessors remains feasible and important [56] [4].
Essential Research Reagent Solutions
Table 4: Key Methodological Tools for Implementing Optimization Techniques
| Tool Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Randomization Tools | Computer-generated random numbers; Interactive Web Response Systems (IWRS); Sealed opaque envelopes | Generate and conceal allocation sequences | Ensuring unpredictable treatment assignment; Maintaining allocation concealment |
| Blinding Tools | Matching placebos; Double-dummy kits; Sham procedures; Centralized outcome assessment | Conceal treatment identity from participants and researchers | Preventing performance and detection bias in clinical trials |
| Statistical Software | R, SAS, SPSS, Stata; Mixed-effects models; Regression procedures; Randomization test macros | Implement complex adjustment methods and analyze trial data | Conducting covariate-adjusted analysis; Handling missing data appropriately |
| Reporting Guidelines | CONSORT checklist; ICH E9 Statistical Principles | Ensure transparent reporting of methods and results | Meeting regulatory standards; Enhancing research reproducibility |
Blinding, randomization, and statistical adjustment represent complementary methodological approaches that together form the foundation of valid experimental research. While each technique addresses specific bias risks, their integrated implementation provides the strongest protection against threats to validity. Randomization establishes the foundation for causal inference by balancing known and unknown confounders [54] [55]. Blinding preserves this balance during trial conduct by preventing differential treatment and assessment [56] [57]. Statistical adjustment then refines the effect estimates during analysis by accounting for any residual imbalances [54] [55].
The choice among these techniques and their specific implementation should be guided by the research context, practical constraints, and the specific bias risks being addressed. By understanding the comparative strengths, limitations, and optimal applications of each method, researchers can design more robust studies that yield reliable evidence, ultimately advancing scientific knowledge and informing evidence-based practice across diverse fields of inquiry.
In human subjects research, the use of placebos represents a critical intersection of methodological rigor and ethical responsibility. Placebo-controlled trials are a cornerstone of clinical research, widely regarded as the "best method for controlling bias in a prospective randomized clinical trial" because they provide the most rigorous test of treatment efficacy [60]. The ethical challenge arises from the tension between the scientific necessity of blinding and controlling for bias, and the moral imperative of fully informing research participants about the nature, risks, and potential benefits of their involvement [60]. This guide examines these ethical considerations within the broader methodological context of experimental versus observational research, comparing key approaches and their implications for researchers, scientists, and drug development professionals.
Experimental vs. Observational Research: A Foundational Comparison
All clinical research operates within two primary methodological paradigms: experimental studies and observational studies. Understanding their fundamental differences is essential for contextualizing the use of placebos.
Table: Comparison of Experimental and Observational Research Designs
| Characteristic | Experimental Studies (e.g., RCTs) | Observational Studies |
|---|---|---|
| Researcher Control | Active manipulation of variables under controlled conditions [4] | No intervention; observation of naturally occurring variables [4] |
| Ability to Establish Causation | High, due to controlled conditions and randomization [4] | Limited, due to potential confounding factors [5] [4] |
| Randomization | Participants randomly assigned to groups [5] | Typically no randomization [4] |
| Key Methodology | Comparison of intervention vs. control (e.g., placebo) groups [5] | Cohort studies, case-control studies [5] |
| Setting | Controlled (e.g., laboratory) [4] | Natural setting [4] |
| Ethical Constraints | May be limited if manipulation poses risk [4] | Often preferred when experimentation is unethical [4] |
Randomized Controlled Trials (RCTs), where one group receives the intervention and a control group receives nothing or an inactive placebo, are considered the "gold standard" for producing reliable evidence of causation [5]. The use of a placebo is a key feature of this experimental design, allowing researchers to control for the natural history of a disease and minimize bias that could result from the research participant or investigator knowing which treatment was received [60].
The Science of Placebo and Nocebo Effects
Placebos are not merely "inert" substances. The placebo effect refers to a "real psychobiological response that results in an objective or subjective benefit," while the nocebo effect refers to a "harmful or dangerous outcome from treatment with an inactive agent" [60]. These effects have documented biological mechanisms. For instance, placebo analgesic effects are associated with the release of endogenous opioids and dopamine, while nocebo pain effects are related to activation of cholecystokinin (CCK) and deactivation of dopamine [60]. The magnitude of these effects can be substantial; in acute postoperative pain, approximately 16% of patients obtained greater than 50% pain relief from a placebo [60].
Biological Pathways of Placebo and Nocebo Effects
Ethical Dilemmas in Placebo-Controlled Trials
The primary ethical conflict lies in the informed consent process. Researchers are ethically obligated to ensure participants understand the "reasonably foreseeable risks and benefits," yet disclosing the potential for placebo or nocebo effects can actually create expectancy that influences these very outcomes [60]. This creates a catch-22 situation where full disclosure may compromise scientific validity, while incomplete disclosure violates the ethical principle of respect for persons.
A review of how placebos are defined in Informed Consent Forms (ICFs) found that the majority of explanations (52.9%) described both the appearance and effects of placebos, while 33.8% defined placebos based on effects alone, and 6.9% described only appearance [61]. Critically, no ICFs in the review contained information about the placebo effect or the potential for nocebo effects or adverse reactions [61].
Table: Analysis of Placebo Definitions in Informed Consent Forms (n=359)
| Definition Type | Frequency | Percentage | Example Description |
|---|---|---|---|
| Appearance and Effects | 190 | 52.9% | "A placebo is a dummy medicine that looks like the real medicine but does not contain any active substance." [61] |
| Effects Only | 121 | 33.8% | "A substance that does not contain active medication." [61] |
| Appearance Only | 25 | 6.9% | "A placebo is a substance that is identical in appearance to the drug being investigated." [61] |
| No Definition | 23 | 6.4% | (Not provided) |
Experimental Protocols and Methodological Variations
Standard Placebo Control Design
The standard placebo control is the most common design. The placebo is designed to be indistinguishable from the active intervention in external characteristics (appearance, taste, smell) but contains no active therapeutic components [62]. The GAP study (Gabapentin in Post-Surgery Pain) exemplifies this approach, describing the placebo as a "dummy pill" in consent documents without mentioning potential placebo/nocebo effects [60].
Standard Placebo-Controlled Trial Workflow
Active Placebo Control Design
Some trials employ an "active placebo" that mimics both the external characteristics and the internal sensations or side effects of the active treatment, without providing therapeutic benefit [62]. This approach is particularly valuable when the experimental drug has perceptible side effects (e.g., dry mouth from tricyclic antidepressants) that could "unblind" participants, potentially introducing bias through expectancy effects [62]. For example, atropine can be used to imitate the anticholinergic effects of tricyclic antidepressants without providing antidepressant action [62].
Table: Comparison of Placebo Types in Clinical Trials
| Characteristic | Standard Placebo | Active Placebo |
|---|---|---|
| Primary Function | Control for external characteristics and natural history [60] [62] | Control for external characteristics AND specific side effects [62] |
| Composition | Inert substance with no known biological effects [60] | Contains an active agent to mimic side effects, but without therapeutic benefit for condition under study [62] |
| Key Advantage | Simplicity and widespread acceptance [60] | Reduces risk of unblinding due to lack of side effects in control group [62] |
| Key Disadvantage | Risk of unblinding if active treatment has perceptible effects [62] | Potential for unintended therapeutic effects or ethical concerns about exposing controls to additional active substances [62] |
| Ideal Use Case | Treatments with no perceptible immediate effects | Treatments with immediate, perceptible psychotropic or adverse effects (e.g., SSRIs, TCAs) [62] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Materials for Placebo-Controlled Trial Implementation
| Item | Function in Research |
|---|---|
| Inert Placebo Formulation | Matches the active drug in appearance, taste, and texture while containing no active pharmaceutical ingredient; serves as the control intervention [60] [61] |
| Active Placebo Compound | For active placebo designs; a substance that mimics specific side effects of the experimental drug without providing therapeutic benefit for the condition being studied (e.g., atropine for anticholinergic effects) [62] |
| Blinding Protocol Materials | Comprehensive documentation and packaging systems to ensure the intervention assignment is concealed from participants, investigators, and outcome assessors [60] [62] |
| Validated Informed Consent Forms | Documents that accurately describe the research, including the use of placebo, probability of assignment to different groups, and potential risks/benefits, while minimizing suggestibility of placebo/nocebo effects [60] [61] |
| Standardized Outcome Measures | Particularly important for subjective endpoints (e.g., pain scales) that are most susceptible to placebo/nocebo effects; enables objective comparison between groups [60] |
Quantitative Analysis of Placebo Reporting Practices
The implementation of ethical principles can be measured through systematic analysis of research documentation. A comprehensive review of 359 research protocols revealed that pharmaceutical companies sponsored the vast majority (91.9%) of placebo-controlled trials, with Phase III studies being most common (59.9%) [61]. The mean length of placebo descriptions in ICFs was notably brief, averaging only 14 words in the original Spanish versions [61].
When analyzed by medical specialty, clinical trials in oncology (15.0%), cardiology (14.2%), and neurology (13.1%) represented the largest proportions of placebo-controlled studies [61]. This distribution reflects the therapeutic areas where placebo controls are most ethically justifiable—typically where no proven intervention exists or where standard treatments are being compared against new interventions with potentially superior efficacy or safety profiles.
The use of placebos in human subjects research remains an essential methodological tool with complex ethical implications. The tension between scientific validity and informed consent requires careful navigation, with approaches ranging from standard placebo controls to more methodologically sophisticated active placebos. Current practice, as documented in consent forms, frequently omits discussion of placebo and nocebo effects, potentially undermining truly informed consent. As research methodologies evolve, the ethical framework governing placebo use must similarly advance, ensuring both scientific integrity and respect for research participants. Researchers must balance these competing demands through transparent communication, methodological rigor, and ongoing ethical reflection.
Weighing the Evidence: A Critical Framework for Comparing and Interpreting Study Findings
In biomedical and environmental research, distinguishing between mere association and true causation represents a critical foundation for scientific inference and practical decision-making. Association occurs when two variables demonstrate a statistical relationship, such that knowing the value of one provides information about the value of the other [63]. Causation, in contrast, signifies that one event or variable is directly responsible for producing another event or outcome—a true cause-and-effect relationship [64]. This distinction is paramount because observing that an event occurs after an exposure does not necessarily mean the exposure caused the event [65]. The fundamental challenge researchers face lies in the fact that while causal relationships demonstrate association, the reverse is not universally true; association does not automatically imply causation [66].
This article examines the strengths and limitations of approaches for establishing causality and identifying associations, framed within the broader context of experimental tests versus natural observation research. For researchers, scientists, and drug development professionals, understanding these methodologies—and when to apply them—is essential for generating robust, actionable evidence. Observational studies can reveal important relationships in real-world settings, but they are susceptible to alternative explanations including chance, bias, and confounding [65]. Experimental studies, particularly randomized controlled trials (RCTs), provide stronger evidence for causality by design, but may raise ethical concerns, face feasibility constraints, or produce results with limited generalizability [67] [64].
Defining Core Concepts and Methodological Frameworks
Association and Correlation: The Foundation of Statistical Relationships
Association is a broad, non-technical term describing any relationship between two variables [66]. Correlation provides a statistical measure of this relationship, quantified by correlation coefficients that describe both the strength and direction of the association [64]. The most common measures include Pearson's correlation coefficient (r), which assesses linear relationships, and Spearman's rank correlation, which evaluates monotonic relationships without assuming linearity [66].
Crucially, correlations can be positive (both variables increase together), negative (one variable increases as the other decreases), or non-existent (no systematic relationship) [64]. However, even strong, statistically significant correlations may be non-causal, arising instead from confounding factors, selection biases, or mere coincidence [68] [66]. For example, the observed correlation between stork populations and human birth rates in Europe illustrates how two variables can be strongly associated without any causal connection, likely influenced instead by underlying socioeconomic or environmental factors [67].
Causation: Establishing Cause-and-Effect Relationships
Causation exists when a change in one variable (the cause) directly produces a change in another variable (the effect) [64]. Establishing causation requires demonstrating that the effect would not have occurred without the cause, a concept formalized in counterfactual theory where causal effects are defined by comparing observed outcomes with the outcomes that would have occurred under different exposure conditions [69].
In practice, individual causal effects cannot be directly observed because we can only observe the outcome under one potential exposure state for each individual [69]. This fundamental limitation necessitates specific methodological approaches to support causal inferences. The European Medicines Agency emphasizes that signals of potential causation (such as adverse event reports) should be considered hypothesis-generating rather than conclusive evidence, requiring further investigation through well-designed studies [65].
Table 1: Key Terminology in Causal Inference
| Term | Definition | Research Importance |
|---|---|---|
| Confounding | Distortion of exposure-outcome relationship by a common cause [63] | Major threat to causal validity in observational studies [69] |
| Collider Bias | Spurious association created by conditioning on a common effect [63] | Can introduce selection bias when inappropriately adjusted for [69] |
| Temporality | Cause must precede effect in time [66] | Necessary but insufficient criterion for causation [67] |
| Counterfactual | The outcome that would have occurred under different exposure [69] | Foundational concept for modern causal inference methods [69] |
Methodological Frameworks for Causal Assessment
Several formal frameworks guide causal assessment in scientific research. Bradford Hill's criteria offer nine considerations for evaluating causal relationships: strength of association, consistency, specificity, temporality, biological gradient, plausibility, coherence, experimental evidence, and analogy [66]. While not a checklist to be rigidly applied, these criteria provide a structured approach for weighing evidence about potential causal relationships [70].
The potential outcomes framework (or counterfactual framework) formalizes causal inference as a missing data problem, aiming to estimate what would have happened to the same individuals under different exposure conditions [69]. This framework has given rise to precise mathematical definitions of causal effects, including the Average Treatment Effect (ATE), Conditional Average Treatment Effect (CATE), and Average Treatment Effect on the Treated (ATT) [71].
Directed Acyclic Graphs (DAGs) provide a visual representation of assumed causal relationships between variables, helping researchers identify appropriate adjustment sets to control confounding while avoiding collider bias [69] [63]. The U.S. Environmental Protection Agency's CADDIS system employs a pragmatic approach to causal assessment in environmental science, emphasizing the comparison of alternative candidate causes to determine which is best supported by the totality of evidence [70].
Causal Inference Framework
Experimental Approaches for Establishing Causality
Randomized Controlled Trials: The Gold Standard
Randomized Controlled Trials (RCTs) represent the most rigorous experimental design for establishing causal relationships. By randomly allocating participants to intervention and control groups, RCTs aim to balance both known and unknown confounding factors, creating comparable groups that differ primarily in their exposure to the intervention [69]. This design minimizes biases and confounding, allowing researchers to attribute outcome differences to the intervention itself rather than extraneous factors [65].
The fundamental strength of RCTs lies in their ability to support strong causal inferences through their design rather than statistical adjustment alone [69]. When properly implemented with adequate sample sizes, concealment of allocation, and blinded outcome assessment, RCTs provide the highest quality evidence for causal relationships in clinical and intervention research.
Table 2: Key Experimental Reagents and Methodological Tools for Causal Inference
| Research Tool | Primary Function | Application Context |
|---|---|---|
| Randomization Protocol | Balances known and unknown confounders across study groups | RCTs to ensure group comparability at baseline [69] |
| Placebo Control | Ispecific effects of intervention from psychological expectations | Clinical trials to maintain blinding and control for placebo effects [68] |
| Blinding Procedures | Prevents ascertainment bias among participants and outcome assessors | Experimental studies to minimize bias in outcome measurement [64] |
| Power Calculation | Determines sample size needed to detect clinically important effects | Study planning to ensure adequate statistical power [66] |
Experimental Protocols and Implementation
Protocol for Parallel-Group Randomized Controlled Trial:
- Define Eligibility Criteria: Establish explicit inclusion and exclusion criteria for the target population [64]
- Sample Size Calculation: Determine required sample size based on expected effect size, alpha error, and statistical power [66]
- Random Allocation: Implement computer-generated random sequence to assign participants to intervention or control groups [69]
- Allocation Concealment: Ensure those enrolling participants cannot foresee assignment to prevent selection bias [64]
- Blinding: Mask participants, intervention administrators, and outcome assessors to group assignment where possible [64]
- Intervention Protocol: Standardize intervention and control conditions with detailed manual of procedures [65]
- Outcome Assessment: Implement validated, objective outcome measures at predefined time points [66]
- Statistical Analysis: Conduct intention-to-treat analysis to preserve randomization benefits [69]
Strengths and Limitations of Experimental Approaches
Experimental approaches, particularly RCTs, offer significant strengths for causal inference but also face important limitations. Their primary strength lies in the high internal validity achieved through random assignment, which minimizes confounding and selection bias [69]. The controlled nature of experiments allows researchers to isolate specific causal effects of interventions while controlling extraneous factors [64]. Furthermore, the blinding procedures possible in many experimental designs reduce measurement and ascertainment biases [64].
However, experimental approaches face ethical constraints when interventions involve potential harm, making them unsuitable for many important research questions [67] [64]. RCTs are often expensive and time-consuming to conduct, particularly for long-term outcomes [67]. The highly controlled conditions may limit generalizability to real-world settings where comorbidities, concomitant treatments, and adherence issues are present [67]. Additionally, participants who consent to randomization may differ from the broader target population, further limiting external validity [69].
Observational Approaches for Identifying Associations
Observational Study Designs
Observational research examines relationships between exposures and outcomes without intervening in the assignment of exposures [67]. These studies can be conducted for various purposes: estimating disease frequency, predicting outcomes, generating hypotheses, or identifying causal relationships [67]. Common observational designs include cohort studies (following exposed and unexposed groups forward in time), case-control studies (comparing exposure histories between cases and controls), and cross-sectional studies (assessing exposure and outcome simultaneously in a population) [67].
In human epidemiological research, 94% of observational studies define specific exposure-outcome pairings of interest, compared to only 21% in veterinary observational studies, suggesting different methodological approaches across disciplines [67]. Observational studies typically rely on statistical adjustment rather than design features to control for confounding, though this requires accurate measurement of all relevant confounders [69].
Statistical Methods for Controlling Confounding
In observational studies, various statistical approaches attempt to address confounding, a situation where an exposure and outcome share a common cause, creating a spurious association between them [63]. Multivariable regression remains the most common approach, simultaneously adjusting for multiple confounders in a statistical model [67]. More advanced methods include propensity score techniques, which create a composite score representing the probability of exposure given observed covariates and then use matching, weighting, or stratification to balance these scores between exposed and unexposed groups [69]. Marginal structural models use inverse probability weighting to control for time-varying confounders that may also be affected by prior exposure [69].
The selection of confounding variables for adjustment should ideally be guided by prior knowledge of causal structures, often represented through Directed Acyclic Graphs (DAGs) [67]. However, in practice, observational studies in veterinary populations use data-driven variable selection methods in 93% of cases, compared to only 16% in human epidemiological studies published in high-impact journals [67].
Observational Research Approaches
Natural Experiments and Quasi-Experimental Designs
Some observational studies leverage natural experiments or quasi-experimental designs that approximate randomization through external circumstances [72]. Regression discontinuity designs exploit situations where an intervention is provided based on whether subjects fall above or below a specific threshold on a continuous variable [69]. By comparing outcomes just above and just below the threshold, researchers can estimate causal effects under the assumption that units near the threshold are comparable except for treatment receipt [69].
Another approach utilizes instrumental variables, which are variables that influence exposure but affect the outcome only through their effect on exposure [69]. When valid instruments are available, they can help control for unmeasured confounding. For example, the Huai River policy in China, which provides winter heating based on geographical location north of the river, has been used as a natural experiment to study the health effects of air pollution [72]. These design-based approaches to causal inference rely less on statistical adjustment and more on identifying contexts that mimic random assignment [69].
Strengths and Limitations of Observational Approaches
Observational studies offer several important advantages, particularly for research questions where experiments are impractical or unethical [67]. They can be conducted using existing data sources, making them more efficient and cost-effective than experimental studies [67]. Observational studies typically include more diverse and representative populations than RCTs, enhancing external validity and generalizability to real-world settings [67]. They are essential for studying rare outcomes or long-term effects that would be impractical to address through experiments [64]. Furthermore, they allow researchers to study multiple exposures and outcomes simultaneously, providing a more comprehensive understanding of complex systems [67].
The primary limitation of observational approaches is their vulnerability to confounding, as unmeasured or imperfectly measured variables can create spurious associations [69] [63]. Selection bias may occur if the process for selecting participants into the study is related to both exposure and outcome [69]. Measurement error can distort observed relationships, particularly if exposure assessment differs between cases and controls [69]. Establishing temporality (ensuring cause precedes effect) can be challenging in some observational designs [67]. Additionally, data-driven analytical approaches common in observational research can increase the probability of biased results and poor replicability [67].
Table 3: Comparison of Approaches for Establishing Causality and Identifying Association
| Characteristic | Experimental Approaches (RCTs) | Observational Approaches | Advanced Causal Inference Methods |
|---|---|---|---|
| Primary Strength | High internal validity through randomization [69] | Broader generalizability and real-world applicability [67] | Balance internal and external validity [69] |
| Key Limitation | Limited generalizability, ethical constraints [67] [64] | Vulnerable to confounding and biases [69] [63] | Require strong assumptions that may be untestable [69] |
| Confounding Control | Design-based (randomization) [69] | Statistical adjustment [69] | Combination of design and statistical methods [69] |
| Implementation Context | Ethical, feasible interventions [64] | Any setting, including existing data [67] | Natural experiments, specific policy contexts [72] |
| Causal Conclusion Strength | Strongest evidence for causation [65] | Weaker evidence, requires careful interpretation [65] | Intermediate, depends on design and assumptions [69] |
Integration and Triangulation: A Modern Approach to Causal Inference
The Triangulation Framework
Given the limitations of any single methodological approach, modern causal inference increasingly emphasizes triangulation—the thoughtful application of multiple approaches with different, largely unrelated sources of potential bias [69]. By integrating evidence from diverse methods (e.g., RCTs, observational studies using different design and statistical approaches, natural experiments), researchers can evaluate whether consistent findings emerge despite different methodological limitations [69]. When results converge across methods with different assumptions and potential biases, confidence in causal conclusions strengthens substantially [69].
Triangulation represents part of wider efforts to improve the transparency and robustness of scientific research, acknowledging that no single method can provide a definitive answer to complex causal questions [69]. This approach is particularly valuable when confronting inconsistent findings or when ethical and practical constraints limit optimal study designs.
Causal Discovery Methods
Causal discovery represents a distinct approach to causal analysis focused on identifying underlying causal structures from observational data [71]. Unlike causal inference, which typically estimates the magnitude of a causal effect for a predefined exposure-outcome relationship, causal discovery aims to uncover the network of causal relationships among multiple variables [71]. Common methods include constraint-based approaches (using conditional independence tests), score-based methods (searching for best-fitting causal graphs), and functional causal models (representing effects as functions of causes plus noise) [71].
These methods can help identify which variables have causal effects on outcomes, potential interventions worth testing, and causal pathways through which variables influence each other [71]. While causal discovery methods cannot definitively establish causation without additional validation, they generate hypotheses for further testing through experimental or quasi-experimental approaches [71].
The choice between approaches for establishing causality versus identifying association depends fundamentally on the research question, ethical considerations, feasibility constraints, and intended use of the results. Experimental methods, particularly RCTs, provide the strongest evidence for causal effects when feasible and ethical to implement [69]. Observational approaches offer valuable insights into real-world relationships and are essential for many research questions where experiments are impractical, but require careful attention to confounding control and interpretation [67].
For researchers and drug development professionals, understanding both the theoretical foundations and practical implementation of these approaches is crucial for designing robust studies and critically evaluating evidence. No single methodology is universally superior; each contributes distinct strengths to the scientific enterprise. The most compelling causal evidence often emerges from the triangulation of multiple methods, each with different assumptions and potential biases, providing convergent evidence for causal relationships [69]. As causal inference methodologies continue to evolve, the integration of design-based and statistical approaches offers promising avenues for strengthening causal conclusions from both experimental and observational research.
The Scientist's Toolkit: Essential Reagent Solutions
The following table details key materials and reagents essential for conducting controlled experimental studies, particularly in biomedical and pharmacological research [4].
| Reagent/Material | Function/Brief Explanation |
|---|---|
| Test Compound/Intervention | The drug, treatment, or variable whose effect is being measured. |
| Placebo | An inactive substance identical in appearance to the test compound, used in control groups to blind the study [5]. |
| Randomization Software/Protocol | A system to ensure random assignment of subjects to control or experimental groups, minimizing selection bias [4]. |
| Blinding Materials | Procedures and labeling to conceal group assignment from participants and/or researchers to prevent bias. |
| Validated Assay Kits | Pre-optimized reagents for quantifying specific biological or biochemical markers (e.g., ELISA for cytokine measurement). |
| Cell Lines or Animal Models | Biological systems used to model human disease or test interventions before human trials [4]. |
| Standardized Data Collection Tools | Electronic Case Report Forms (eCRFs) or other tools to ensure consistent and accurate data capture across all study sites. |
Experimental vs. Observational Studies: A Structured Analysis
The choice between experimental and observational study designs is fundamental to research integrity. The table below provides a head-to-head comparison of these two methodologies [5] [4].
| Comparison Criteria | Experimental Studies | Observational Studies |
|---|---|---|
| Researcher Control Over Variables | Active manipulation of independent variables under controlled conditions [4]. | No direct manipulation; observation of variables as they occur naturally [4]. |
| Primary Research Goal | To establish cause-and-effect relationships [4]. | To identify patterns, associations, and generate hypotheses [5] [4]. |
| Ability to Establish Causation | High, due to controlled conditions and randomization [4]. | Limited, as observed associations may be influenced by confounding factors [5] [4]. |
| Randomization of Subjects | Participants are randomly assigned to groups (e.g., control vs. treatment) [5] [4]. | Typically, no randomization; subjects are observed in pre-existing groups [4]. |
| Setting | Often conducted in controlled laboratory or clinical settings [4]. | Conducted in natural, real-world settings [4]. |
| Key Strengths | Considered the "gold standard" for providing reliable evidence of efficacy; minimizes confounding bias [5] [4]. | Ideal for studying long-term effects, rare events, and situations where experiments are unethical or impractical [5] [4]. |
| Key Limitations | Can be time-consuming, expensive, and may lack generalizability (external validity); not suitable for all research questions [5] [4]. | Results are open to dispute due to potential confounding biases; cannot definitively prove causation [5] [4]. |
| Ethical Considerations | Manipulation may be unethical if it could harm participants [4]. | Often provides an ethical alternative for studying harmful exposures [4]. |
Detailed Methodologies for Key Experiments
Protocol for a Randomized Controlled Trial (RCT)
The RCT is the quintessential experimental study design [5].
- Hypothesis & Definition: Formulate a precise hypothesis. Define the primary outcome variable (e.g., reduction in tumor size) and select the intervention (e.g., a new drug compound).
- Participant Selection: Recruit eligible participants based on predefined inclusion/exclusion criteria. Obtain informed consent.
- Randomization & Blinding: Randomly assign participants to either the intervention group (receives the drug) or the control group (receives a placebo or standard treatment). Use a computer-generated sequence to ensure allocation concealment. Implement blinding (single-, double-, or triple-blind) so that participants and/or investigators are unaware of group assignments [4].
- Intervention & Follow-up: Administer the drug or placebo according to a fixed protocol and schedule. Monitor all participants for a predetermined period.
- Outcome Assessment: Measure the primary and secondary outcomes at the end of the follow-up period using validated tools and assays.
- Data Analysis: Compare outcomes between the intervention and control groups using statistical tests (e.g., t-tests, ANOVA) to determine if observed differences are statistically significant [4].
Protocol for a Cohort Study
A cohort study is a primary type of observational study [5].
- Cohort Definition: Identify and enroll a group of individuals (the cohort) who are linked by a common characteristic or exposure [5].
- Exposure Assessment: Determine the exposure status of each participant (e.g., exposed to a potential environmental risk factor vs. not exposed) at the start of the study. This is not manipulated by the researcher.
- Follow-up: Follow the cohort over a period of time (which can be years or decades) to track the development of specific outcomes or diseases [4].
- Outcome Measurement: Identify and record the incidence of the outcome of interest in both the exposed and non-exposed groups.
- Data Analysis & Confounding Control: Calculate and compare the risk of the outcome between groups. Use statistical techniques like regression analysis to control for potential confounding factors (e.g., age, diet, lifestyle) [4].
Visualizing Research Methodologies
The following diagrams illustrate the logical workflows for the core research methodologies discussed.
RCT Experimental Workflow
Observational Cohort Workflow
In the pursuit of scientific knowledge, researchers navigate two distinct pathways: the controlled manipulation of experiments and the naturalistic observation of real-world phenomena. Experimental studies, particularly Randomized Controlled Trials (RCTs), are revered as the "gold standard" for establishing cause-and-effect relationships through direct intervention and control [2] [1]. In contrast, observational studies glean insights by monitoring subjects without interference, offering a window into effects in natural settings [2] [4]. For researchers and drug development professionals, understanding when these two pillars of evidence converge to reinforce a finding, or diverge to reveal complexity, is critical for advancing medical knowledge and patient care. This guide objectively compares these methodologies, examining their respective strengths, protocols, and the interpretive challenges that arise from their data.
Defining the Methodologies: Core Principles and Procedures
The fundamental distinction between these studies lies in the researcher's role: as an active intervener in experiments, or a passive recorder in observational research [1] [4].
The Experimental Protocol: Establishing Causality
Experimental studies are designed to test specific hypotheses about cause-and-effect relationships by actively manipulating one or more independent variables and observing the impact on a dependent variable [1].
- Core Protocol for a Randomized Controlled Trial (RCT):
- Hypothesis Formulation: Define a clear, predictive statement (e.g., "Drug X reduces systolic blood pressure by a statistically significant amount compared to a placebo").
- Participant Recruitment: Identify a sample population based on specific inclusion and exclusion criteria [2].
- Randomization: Assign participants randomly to either an experimental group (receives the intervention) or a control group (receives a placebo or standard treatment). This minimizes selection bias and distributes confounding factors evenly [2] [1].
- Blinding (Single/Double): Implement blinding so participants (single-blind) or both participants and researchers (double-blind) do not know group assignments to prevent bias [2].
- Intervention: Administer the intervention to the experimental group under strictly controlled conditions.
- Data Collection: Measure the outcome variable(s) (e.g., blood pressure) across all groups at specified time points.
- Data Analysis: Use inferential statistics (e.g., t-tests, ANOVA) to determine if outcome differences between groups are statistically significant [4].
The Observational Protocol: Discovering Correlations
Observational studies investigate associations and patterns where experimentation is impractical or unethical. The researcher measures variables of interest without manipulating them [1] [4].
- Core Protocol for a Cohort Study:
- Research Question: Formulate a question about a potential risk or benefit (e.g., "Does prolonged smartphone use increase the risk of eye strain?").
- Cohort Selection: Identify a group of participants who do not have the outcome of interest and classify them based on their exposure (e.g., high vs. low smartphone use) [2].
- Follow-up: Observe the cohorts over a period of time (this can be prospective or retrospective) [2].
- Data Collection: Record the incidence of the outcome (e.g., diagnosis of eye strain) in both exposed and non-exposed groups.
- Data Analysis: Calculate and compare the risk of developing the outcome between the groups, often using measures like relative risk [2].
Direct Comparison: Strengths, Weaknesses, and Applications
The choice between an experimental and observational design involves trade-offs between control, real-world applicability, and the ability to prove causation. The table below summarizes these key differences.
Table 1: Comparative Analysis of Experimental and Observational Study Designs
| Aspect | Experimental Study | Observational Study |
|---|---|---|
| Primary Objective | Establish cause-and-effect relationships [1] [4] | Identify associations and patterns [1] |
| Researcher Control | High control; variables are manipulated [1] | No direct manipulation of variables [4] |
| Variable Manipulation | Active manipulation of independent variable(s) [1] | Observation of naturally occurring variables [4] |
| Randomization | Participants are randomly assigned to groups [2] [1] | No randomization; subjects are observed in pre-existing groups [4] |
| Setting | Controlled (e.g., laboratory) [1] [4] | Naturalistic (real-world environment) [1] [4] |
| Key Strength | High internal validity; can establish causality [1] | High ecological validity; studies ethically complex issues [2] [1] |
| Key Limitation | Can lack ecological validity; may be unethical for some risks [1] | Susceptible to confounding variables; cannot prove causation [2] [1] |
| Ideal Application | Testing efficacy of a new drug or specific intervention [2] | Studying long-term health risks, disease progression, or rare events [4] |
Convergence and Divergence: Interpreting the Evidence
The true test of a scientific hypothesis often comes when evidence from both experimental and observational streams can be compared.
Table 2: Scenarios of Convergence and Divergence Between Study Types
| Scenario | Implications for Research | Example in Drug Development |
|---|---|---|
| Convergence | Findings from both methods align, providing strong, multi-faceted evidence that enhances generalizability and confidence in the result [4]. | An RCT shows a drug reduces heart attack risk, and a large prospective cohort study confirms a correlation between the drug's use and lower real-world incidence [73]. |
| Divergence | Experimental and observational results conflict. This signals potential confounding factors, bias in the observational study, or limited generalizability of the experimental findings [1]. | Observational studies suggest a vitamin supplement is beneficial, but a rigorous RCT finds no effect beyond placebo, indicating a healthy-user bias in the observational data [1]. |
| Integration | Observational studies generate hypotheses about new therapeutic uses for existing drugs, which are then validated through targeted RCTs, creating an efficient discovery pipeline [73] [4]. | Real-World Evidence (RWE) from patient records is used to support regulatory submissions for label expansions, complementing initial RCT data [73]. |
The Scientist's Toolkit: Essential Reagents and Materials
The integrity of both experimental and observational research hinges on the quality of materials and methods. Below is a non-exhaustive list of key reagents and tools.
Table 3: Essential Research Reagent Solutions for Clinical Studies
| Item/Category | Function in Research |
|---|---|
| Placebo | An inert substance identical in appearance to the investigational product, used in the control group of an RCT to blind participants and isolate the drug's specific effect from the placebo effect [2]. |
| Investigational Product | The drug, biologic, or device being studied. Its manufacturing must adhere to Good Manufacturing Practice (GMP) to ensure consistent quality and purity throughout the trial [73]. |
| Binding Agents & Fillers | Inactive ingredients (excipients) used in drug formulation to provide bulk, stability, and controlled release of the active pharmaceutical ingredient (API). |
| Clinical Outcome Assessment (COA) | A standardized tool or instrument (e.g., questionnaire, lab test, wearable sensor) used to measure a patient's health status, symptom severity, or physical performance [2]. |
| Data from Electronic Health Records (EHR) | In observational studies, EHRs provide a source of Real-World Data (RWD) on patient diagnoses, treatments, and outcomes outside the controlled clinical trial setting [73]. |
Visualizing Research Pathways and Decision-Making
The following diagrams, created using the specified color palette, map out the logical flow of research methodologies and the decision process for selecting the appropriate study type.
Research Method Decision Tree
Integrating Evidence for Decision-Making
The dichotomy between observational and experimental studies is not a contest for supremacy, but a framework for building robust and clinically relevant knowledge. While the RCT remains the gold standard for establishing efficacy under ideal conditions, the rich, real-world context provided by observational studies is increasingly valued, particularly as regulatory bodies like the FDA and EMA develop frameworks for integrating Real-World Evidence into submissions [73]. For today's researcher, the most powerful strategy is a synergistic one—using these methods not in opposition, but in concert. By understanding their points of convergence and divergence, scientists can construct a more complete and actionable evidence base, ultimately accelerating the development of safe and effective treatments for patients worldwide.
In the pursuit of scientific knowledge, researchers often face a fundamental methodological choice: to implement controlled experimental tests or to observe phenomena through natural observation research. Experimental tests, such as Randomized Controlled Trials (RCTs), provide high internal validity through controlled conditions and random assignment, establishing causal inference with considerable reliability [74]. In contrast, naturalistic observation and Natural Experiments (NEs) study subjects in their real-world environments without interference, offering high ecological validity and suitability for contexts where experimental manipulation is impractical or unethical [35] [74]. Systematic reviews and meta-analyses represent the pinnacle of evidence synthesis, rigorously combining findings across this methodological spectrum to provide comprehensive, unbiased conclusions about what truly works in healthcare and beyond [75] [76].
The following diagram illustrates the foundational relationship between primary research methodologies and the evidence synthesis process they feed into.
Methodological Foundations: Systematic Reviews vs. Meta-Analysis
A systematic review is a research method that involves a detailed and comprehensive plan and search strategy derived a priori, with the goal of reducing bias by systematically identifying, appraising, and synthesizing all relevant studies on a particular topic [75]. Systematic reviews differ from traditional narrative reviews, which are often descriptive and can include selection bias, by employing a reproducible, rigorous methodology [75].
A meta-analysis is a statistical component often included in systematic reviews, which involves synthesizing quantitative data from several studies into a single quantitative estimate or summary effect size [75]. This synthesis provides more precise estimates of effects and allows for the exploration of heterogeneity across studies. Table 1 outlines the key stages of conducting a systematic review and meta-analysis.
Table 1: The 8 Key Stages of a Systematic Review and Meta-Analysis [75]
| Stage | Key Activities | Outputs/Considerations |
|---|---|---|
| 1. Formulate Question | Define review question, form hypotheses, develop title (Intervention for population with condition). | PICOS framework (Population, Intervention, Comparison, Outcomes, Study types). |
| 2. Define Criteria | Define explicit inclusion/exclusion criteria for studies. | Decisions on population age/condition, interventions, comparators, outcomes, study designs (e.g., RCTs only), publication status. |
| 3. Search Strategy | Develop comprehensive search strategy with librarian help. | Balance sensitivity/ specificity; use databases, reference lists, journals, listservs, experts. |
| 4. Select Studies | Screen abstracts/full texts against criteria. | At least two reviewers for reliability; log of decisions; contact authors for missing data. |
| 5. Extract Data | Use standardized form to extract data from included studies. | Data on authors, year, participants, design, outcomes; two reviewers to minimize error. |
| 6. Assess Study Quality | Critically appraise methodological quality of each study. | Use scales (e.g., Jadad) or guidelines (e.g., CONSORT); consider appropriateness for intervention type. |
| 7. Analyze & Interpret | Synthesize data statistically (meta-analysis) and interpret findings. | Calculate effect sizes (SMD, OR, RR) with confidence intervals; forest plots; assess heterogeneity; provide clinical/research recommendations. |
| 8. Disseminate Findings | Publish and disseminate the review. | Publish in journals (e.g., Cochrane Database); create plain language summaries; plan for future updates. |
Comparative Analysis: Synthesizing Experimental and Naturalistic Evidence
Systematic reviews powerfully integrate findings from both experimental and naturalistic research paradigms. Table 2 compares these primary study designs, highlighting their distinct advantages and challenges for inclusion in evidence synthesis.
Table 2: Comparison of Primary Study Types for Evidence Synthesis [75] [35] [76]
| Characteristic | Experimental Tests (e.g., RCTs) | Natural Observation (e.g., Natural Experiments) |
|---|---|---|
| Definition | Study where the investigator actively controls and manipulates the intervention, with random assignment to groups. | Study of subjects in their natural environment without any intervention or manipulation by the investigator. |
| Intervention/Exposure Assignment | Controlled by the researcher; random allocation. | Not controlled by the researcher; occurs through natural processes or policy changes. |
| Control for Confounding | High; randomization balances known and unknown confounders (in expectation). | Variable; confounding due to selective exposure must be addressed by design (e.g., DiD, IV) and analysis. |
| Internal Validity | High. | Can be strengthened with rigorous methods but is often lower than RCTs. |
| Ecological Validity | Can be lower, as lab settings may not reflect real world. | High, as behaviors are studied in authentic, real-world settings. |
| Key Analysis Methods | Group comparison (t-tests, ANOVA). | Difference-in-Differences (DiD), Interrupted Time Series (ITS), Regression Discontinuity (RD). |
| Causal Inference Strength | Strong for effects of assignment (Intention-to-Treat). | Possible with careful design, but often context-dependent (e.g., Local Average Treatment Effects). |
| Primary Strengths | Gold standard for establishing causality. | Suitable for topics unethical or impractical for labs; reveals real-world behavior and policy impacts. |
| Primary Limitations | Can be expensive, time-consuming; may lack generalizability. | Lack of control introduces risk of bias and confounding; causal inference is less straightforward. |
| Role in Evidence Synthesis | Often considered highest quality evidence; primary input for many meta-analyses. | Provides crucial real-world context and evidence on interventions not testable in trials. |
Experimental Protocols and Advanced Meta-Analysis Techniques
The Systematic Review Protocol
A rigorous systematic review is based on a predefined, detailed protocol that ensures transparency and reproducibility, minimizing bias and enhancing the reliability of the findings [76]. This protocol, often registered with organizations like the Cochrane Collaboration, outlines the planned methods including the search strategy, inclusion criteria, and data analysis plan before the review begins [75].
Meta-Analysis Statistical Workflow
The core of a meta-analysis involves a specific statistical workflow to calculate a summary effect from multiple studies. Different statistical methods can be employed, including the weighted average method (where the weight is usually the inverse of the variance of the effect size), Peto method (for rare events), and random-effects meta-regression (which accounts for between-study variance) [76]. The process of statistically synthesizing this data is visualized below.
The Scientist's Toolkit: Essential Reagents for Evidence Synthesis
Conducting a high-quality systematic review requires more than just scholarly diligence; it relies on a suite of methodological tools and software solutions. The following table details key resources in the modern systematic reviewer's toolkit.
Table 3: Essential Toolkit for Conducting Systematic Reviews and Meta-Analyses [75] [77]
| Tool/Resource Category | Specific Examples | Function & Application |
|---|---|---|
| Protocol & Reporting Guidelines | Cochrane Handbook, PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement | Provide standardized frameworks for planning, conducting, and reporting reviews to ensure methodological rigor and completeness. |
| Reference Management Software | EndNote, Zotero, Mendeley | Facilitate storage, organization, deduplication, and citation of thousands of retrieved study records. |
| Systematic Review Software | Covidence, Rayyan | Streamline the screening and selection process with blind duplicate review, conflict resolution, and decision logging. |
| Statistical Analysis Platforms | R (metafor, meta packages), Stata (metan), RevMan (Cochrane's Review Manager) | Perform meta-analyses, calculate effect sizes and confidence intervals, generate forest and funnel plots, and assess heterogeneity. |
| Data Visualization Tools | R (ggplot2), Python (Matplotlib, Seaborn), Datylon | Create publication-ready visualizations like forest plots, risk-of-bias assessments, and PRISMA flow diagrams. |
| Bias Assessment Tools | Cochrane Risk of Bias (RoB 2) tool, ROBINS-I, Newcastle-Ottawa Scale | Critically appraise the methodological quality and risk of bias in individual included studies (RCTs and non-RCTs, respectively). |
Limitations and Best Practices in Evidence Synthesis
While powerful, systematic reviews and meta-analyses are not a panacea. Their quality is intrinsically tied to the quality of the primary studies they include; flawed or biased primary studies will lead to a synthesis that reflects those limitations [76]. Other significant challenges include:
- Publication Bias: The tendency for studies with significant or positive results to be more likely published, leading to an overrepresentation of certain findings and a skewed evidence base [76].
- Heterogeneity: Clinical and methodological differences between studies can create heterogeneity. While this can be quantified (e.g., with the I² statistic), significant heterogeneity can complicate the interpretation of a single summary effect [75] [76].
- Dependence on Available Data: The review can only synthesize evidence from studies that have been conducted and are accessible, which may leave gaps in the evidence for specific sub-populations or outcomes.
To mitigate these limitations and ensure robustness, researchers should adhere to best practices: pre-registering their protocol, conducting exhaustive searches (including grey literature), rigorously assessing study quality and risk of bias, transparently reporting all methods and findings (e.g., following PRISMA), and interpreting results with caution, acknowledging the limitations of the underlying evidence [75] [76]. By doing so, systematic reviews and meta-analyses remain the most reliable method for integrating knowledge from both the controlled environment of the experiment and the complex reality of the natural world.
Conclusion
The choice between experimental and observational studies is not a matter of one being universally superior, but rather of selecting the right tool for the specific research question, ethical context, and practical constraints. While RCTs provide the strongest evidence for causality, well-designed observational studies are indispensable for exploring long-term outcomes, rare events, and real-world effectiveness. The future of robust clinical research lies in recognizing the complementary strengths of both methodologies. Embracing a mixed-methods approach, where observational studies generate hypotheses and experimental designs test them, will lead to more nuanced, generalizable, and impactful scientific discoveries. Furthermore, ongoing methodological refinements aimed at minimizing bias in observational studies will continue to narrow the perceived gap in evidence quality, enriching the entire biomedical research landscape.
References
- 1. Experiment vs Observational Study: Similarities & Differences [https://helpfulprofessor.com/experiment-vs-observational-study/]
- 2. Observational vs Experimental Study: Differences & Uses [https://www.allclinicaltrials.com/blog/observational-vs-experimental-studies]
- 3. Quantitative Data Analysis. A Complete Guide [2025] [https://www.6sigma.us/six-sigma-in-focus/quantitative-data-analysis/]
- 4. Observational Study vs Experiment [https://www.uopeople.edu/blog/observational-study-vs-experiment/]
- 5. Observational vs. experimental studies [https://www.iwh.on.ca/what-researchers-mean-by/observational-vs-experimental-studies]
- 6. Quasi-experiment [https://en.wikipedia.org/wiki/Quasi-experiment]
- 7. An Introduction to the Quasi-Experimental Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11741180/]
- 8. Independent vs. Dependent Variables | Definition & ... [https://www.scribbr.com/methodology/independent-and-dependent-variables/]
- 9. Independent vs Dependent Variables | Definition & Examples [https://www.simplypsychology.org/variables.html]
- 10. Dependent Variable [https://www.ncsu.edu/labwrite/po/dependentvar.htm]
- 11. Confounding Variables | Definition, Examples & Controls [https://www.enago.com/academy/confounding-variables/]
- 12. Understanding Confounding Variables [https://amplitude.com/explore/experiment/confounding-variables]
- 13. Independent Variables in Research: A Comprehensive Guide [https://innerview.co/blog/understanding-independent-variables-definition-types-and-examples]
- 14. Independent and Dependent Variables in Research [https://imotions.com/blog/learning/best-practice/roles-of-independent-and-dependent-variables-in-research/?srsltid=AfmBOopeGUJrgzlzl8dO4qAqkltDFecS7MU4v6pAq12hcz_GdHJUvdRm]
- 15. cohort, cross sectional, and case-control studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC1726024/]
- 16. Observational Studies: Cohort and Case-Control Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC2998589/]
- 17. Study designs [https://www.cebm.ox.ac.uk/resources/ebm-tools/study-designs]
- 18. In brief: What types of studies are there? - InformedHealth.org [https://www.ncbi.nlm.nih.gov/books/NBK390304/]
- 19. Observational research methods—Cohort studies, cross ... [https://www.sciencedirect.com/science/article/pii/S2211419X11001637]
- 20. Types of clinical trials [https://www.cancerresearchuk.org/about-cancer/find-a-clinical-trial/what-clinical-trials-are/types-of-clinical-trials]
- 21. Observational Study Designs [https://www.irvinginstitute.columbia.edu/observational-study-designs]
- 22. Study Design Comparison: Quick Reference for Authors [https://pubrica.com/academy/research/comparison-of-cross-sectional-prospective-cohort-study-retrospective-case-control-study-a-quick-reference-table-for-the-authors-researchers/]
- 23. Glossary of Study Designs [https://www.andeal.org/study-designs]
- 24. Randomized controlled trials: Overview, benefits, and ... [https://www.medicalnewstoday.com/articles/280574]
- 25. Strengths and Limitations of RCTs - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK584466/]
- 26. Rethinking the pros and cons of randomized controlled trials ... [https://bmcproc.biomedcentral.com/articles/10.1186/s12919-023-00285-8]
- 27. Large simple randomized controlled trials—from drugs to ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-08724-x]
- 28. Randomized controlled trials vs . observational studies: why not just... [https://bmcanesthesiol.biomedcentral.com/articles/10.1186/s12871-016-0265-3]
- 29. Smarter Trial Designs for Rare Neurological Disease Trials [https://tfscro.com/resources/rare-neurological-disease-trials-smarter-design-with-natural-history-external-controls-and-real-world-evidence/]
- 30. Alternative and Confirmatory Data - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK609394/]
- 31. Randomized controlled trials – The what, when, how and why [https://www.sciencedirect.com/science/article/pii/S147751312400617X]
- 32. effectiveness and safety of pharmaceuticals assessed in... Comparative [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647453/]
- 33. Experimental vs Observational Studies: Differences & ... [https://www.questionpro.com/blog/experimental-vs-observational-studies/]
- 34. How does an observational study differ from an experiment? [https://www.scribbr.co.uk/faqs/observational-study-vs-experiment/]
- 35. Naturalistic Observation | Definition, Guide, & Examples [https://www.scribbr.com/methodology/naturalistic-observation/]
- 36. Observation Methods: Naturalistic, Participant and Controlled [https://www.simplypsychology.org/observation.html]
- 37. Observational vs Experimental Studies Explained [https://www.assignnmentinneed.com/blog/what-is-the-difference-between-an-observational-study-and-experimental-studies]
- 38. Quantitative research: Methods, types & real case studies [https://www.lyssna.com/blog/types-of-quantitative-research/]
- 39. Top Functional Service Providers (FSPs) in Clinical ... [https://www.precisionformedicine.com/blog/top-functional-service-providers-fsps-in-clinical-research-for-2025]
- 40. Top 10 CROs to Watch in 2025 [https://www.proclinical.com/blogs/2025-3/top-10-cros-to-watch-in-2025]
- 41. Dealing with confounding in observational studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10578949/]
- 42. Appropriate design of research and statistical analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC3766773/]
- 43. Avoiding Bias in Observational Studies: Part 8 in a Series ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2780010/]
- 44. Risk of bias in observational studies using routinely collected ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-02151-w]
- 45. Confounding [https://catalogofbias.org/biases/confounding/]
- 46. What Is Selection Bias? | Definition & Examples [https://www.scribbr.com/research-bias/selection-bias/]
- 47. Confounding in Observational Studies Evaluating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8786092/]
- 48. Selection bias [https://catalogofbias.org/biases/selection-bias/]
- 49. Limitations of Experimental Research Design [https://insight7.io/limitations-of-experimental-research-design/]
- 50. Experimental designs used for optimising the effects of health ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-025-13184-9]
- 51. Quasi-Experimental Design Disadvantages [https://pubrica.com/insights/experimental-methodology/quasi-experimental-design-disadvantages/]
- 52. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 53. Quantitative Data Analysis Methods & Techniques 101 [https://gradcoach.com/quantitative-data-analysis-methods/]
- 54. Randomization, blinding, and coding - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK305495/]
- 55. A roadmap to using randomization in clinical trials [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01303-z]
- 56. Blinding in Clinical Trials: Seeing the Big Picture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8308085/]
- 57. Blinding: Who, what, when, why, how? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2947122/]
- 58. Blinding in pharmaceutical clinical trials: An overview of ... [https://www.sciencedirect.com/science/article/abs/pii/S1551714415300185]
- 59. Blinding and Randomization [https://link.springer.com/chapter/10.1007/164_2019_279]
- 60. Informed Consent for Placebo-Controlled Trials: Do Ethics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9841466/]
- 61. The Definition of Placebo in the Informed Consent Forms of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0113654]
- 62. Active placebo versus standard placebo control interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7388745/]
- 63. Association or causation? How do we ever know? [https://catalogofbias.org/2019/03/05/association-or-causation-how-do-we-ever-know/]
- 64. Correlation and causation [https://www.abs.gov.au/statistics/understanding-statistics/statistical-terms-and-concepts/correlation-and-causation]
- 65. What Is the Difference Between Observed Association and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7879446/]
- 66. The difference between association, correlation and ... [https://ledidi.com/academy/the-difference-between-association-correlation-and-causation]
- 67. What question are we trying to answer? Embracing causal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11149352/]
- 68. Understanding Association Versus Causation [https://sudc.org/being-a-critical-consumer-of-medical-research-understanding-association-versus-causation/]
- 69. Causal inference with observational data [https://pmc.ncbi.nlm.nih.gov/articles/PMC8020490/]
- 70. About Causal Assessment | US EPA [https://www.epa.gov/caddis/about-causal-assessment]
- 71. Causal analysis overview: Causal inference versus ... [https://medium.com/data-science-at-microsoft/causal-analysis-overview-causal-inference-versus-experimentation-versus-causal-discovery-d7c4ca99e3e4]
- 72. Causal effects estimation: Using natural experiments in ... [https://www.sciencedirect.com/science/article/pii/S2950362025000098]
- 73. Regulatory strategy reimagined: Three trends accelerating ... [https://www.drugdiscoverytrends.com/regulatory-strategy-reimagined-three-trends-accelerating-drug-development/]
- 74. Natural Experiments: An Overview of Methods, Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6485604/]
- 75. Systematic Reviews and Meta-Analyses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3024725/]
- 76. Systematic review and meta-analysis in clinical trials [https://www.sciencedirect.com/science/article/abs/pii/S1357303925000775]
- 77. Meaningful Product Experimentation: 5 Impactful Data ... [https://www.montecarlodata.com/blog-product-experimentation/]